
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Basic Research
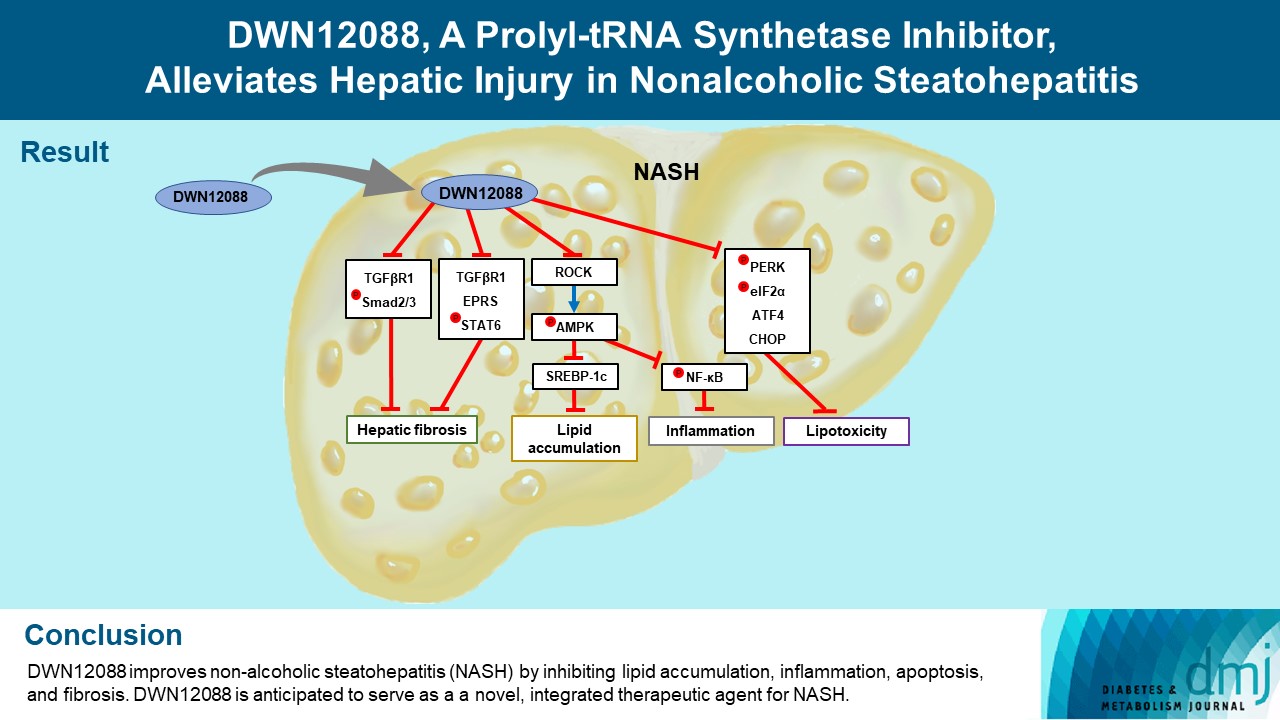
- DWN12088, A Prolyl-tRNA Synthetase Inhibitor, Alleviates Hepatic Injury in Nonalcoholic Steatohepatitis
- Dong-Keon Lee, Su Ho Jo, Eun Soo Lee, Kyung Bong Ha, Na Won Park, Deok-Hoon Kong, Sang-In Park, Joon Seok Park, Choon Hee Chung
- Diabetes Metab J. 2024;48(1):97-111. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0367
- 1,740 View
- 180 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Nonalcoholic steatohepatitis (NASH) is a liver disease caused by obesity that leads to hepatic lipoapoptosis, resulting in fibrosis and cirrhosis. However, the mechanism underlying NASH is largely unknown, and there is currently no effective therapeutic agent against it. DWN12088, an agent used for treating idiopathic pulmonary fibrosis, is a selective prolyl-tRNA synthetase (PRS) inhibitor that suppresses the synthesis of collagen. However, the mechanism underlying the hepatoprotective effect of DWN12088 is not clear. Therefore, we investigated the role of DWN12088 in NASH progression.
Methods
Mice were fed a chow diet or methionine-choline deficient (MCD)-diet, which was administered with DWN12088 or saline by oral gavage for 6 weeks. The effects of DWN12088 on NASH were evaluated by pathophysiological examinations, such as real-time quantitative reverse transcription polymerase chain reaction, immunoblotting, biochemical analysis, and immunohistochemistry. Molecular and cellular mechanisms of hepatic injury were assessed by in vitro cell culture.
Results
DWN12088 attenuated palmitic acid (PA)-induced lipid accumulation and lipoapoptosis by downregulating the Rho-kinase (ROCK)/AMP-activated protein kinase (AMPK)/sterol regulatory element-binding protein-1c (SREBP-1c) and protein kinase R-like endoplasmic reticulum kinase (PERK)/α subunit of eukaryotic initiation factor 2 (eIF2α)/activating transcription factor 4 (ATF4)/C/EBP-homologous protein (CHOP) signaling cascades. PA increased but DWN12088 inhibited the phosphorylation of nuclear factor-κB (NF-κB) p65 (Ser536, Ser276) and the expression of proinflammatory genes. Moreover, the DWN12088 inhibited transforming growth factor β (TGFβ)-induced pro-fibrotic gene expression by suppressing TGFβ receptor 1 (TGFβR1)/Smad2/3 and TGFβR1/glutamyl-prolyl-tRNA synthetase (EPRS)/signal transducer and activator of transcription 6 (STAT6) axis signaling. In the case of MCD-diet-induced NASH, DWN12088 reduced hepatic steatosis, inflammation, and lipoapoptosis and prevented the progression of fibrosis.
Conclusion
Our findings provide new insights about DWN12088, namely that it plays an important role in the overall improvement of NASH. Hence, DWN12088 shows great potential to be developed as a new integrated therapeutic agent for NASH.
- Drug Regimen
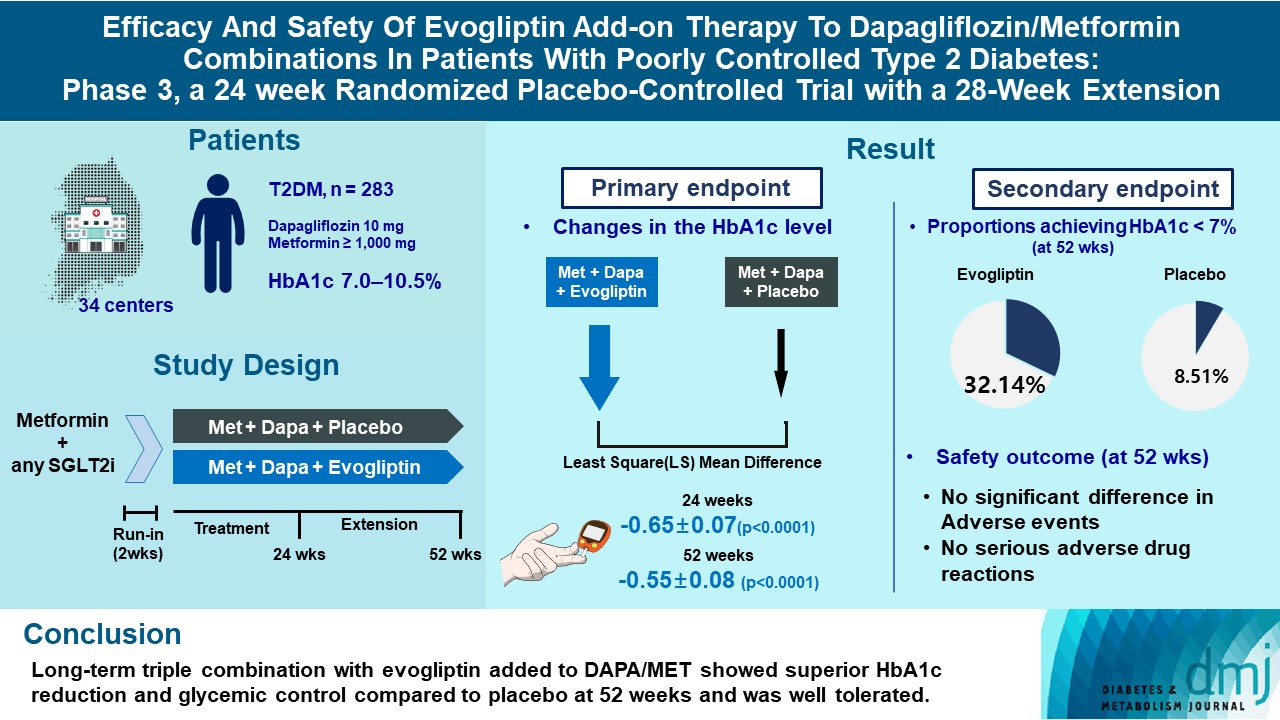
- Efficacy and Safety of Evogliptin Add-on Therapy to Dapagliflozin/Metformin Combinations in Patients with Poorly Controlled Type 2 Diabetes Mellitus: A 24-Week Multicenter Randomized Placebo-Controlled Parallel-Design Phase-3 Trial with a 28-Week Extension
- Jun Sung Moon, Il Rae Park, Hae Jin Kim, Choon Hee Chung, Kyu Chang Won, Kyung Ah Han, Cheol-Young Park, Jong Chul Won, Dong Jun Kim, Gwan Pyo Koh, Eun Sook Kim, Jae Myung Yu, Eun-Gyoung Hong, Chang Beom Lee, Kun-Ho Yoon
- Diabetes Metab J. 2023;47(6):808-817. Published online September 26, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0387
- 2,569 View
- 281 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study investigates the long-term efficacy and safety of evogliptin add-on therapy in patients with inadequately controlled type 2 diabetes mellitus (T2DM) previously received dapagliflozin and metformin (DAPA/MET) combination.
Methods
In this multicenter randomized placebo-controlled phase 3 trial, patients with glycosylated hemoglobin (HbA1c) levels 7.0% to 10.5% (n=283) previously used DAPA 10 mg plus MET (≥1,000 mg) were randomly assigned to the evogliptin 5 mg once daily or placebo group (1:1). The primary endpoint was the difference in the HbA1c level from baseline at week 24, and exploratory endpoints included the efficacy and safety of evogliptin over 52 weeks (trial registration: ClinicalTrials.gov NCT04170998).
Results
Evogliptin add-on to DAPA/MET therapy was superior in HbA1c reduction compared to placebo at weeks 24 and 52 (least square [LS] mean difference, –0.65% and –0.55%; 95% confidence interval [CI], –0.79 to –0.51 and –0.71 to –0.39; P<0.0001). The proportion of patients achieving HbA1c <7% was higher in the triple combination group at week 52 (32.14% vs. 8.51% in placebo; odds ratio, 5.62; P<0.0001). Evogliptin significantly reduced the fasting glucose levels and mean daily glucose levels with improvement in homeostatic model assessment of β-cell function (LS mean difference, 9.04; 95% CI, 1.86 to 16.21; P=0.0138). Adverse events were similar between the groups, and no serious adverse drug reactions were reported in the evogliptin group.
Conclusion
Long-term triple combination with evogliptin added to DAPA/MET showed superior HbA1c reduction and glycemic control compared to placebo at 52 weeks and was well tolerated.
- Basic Research
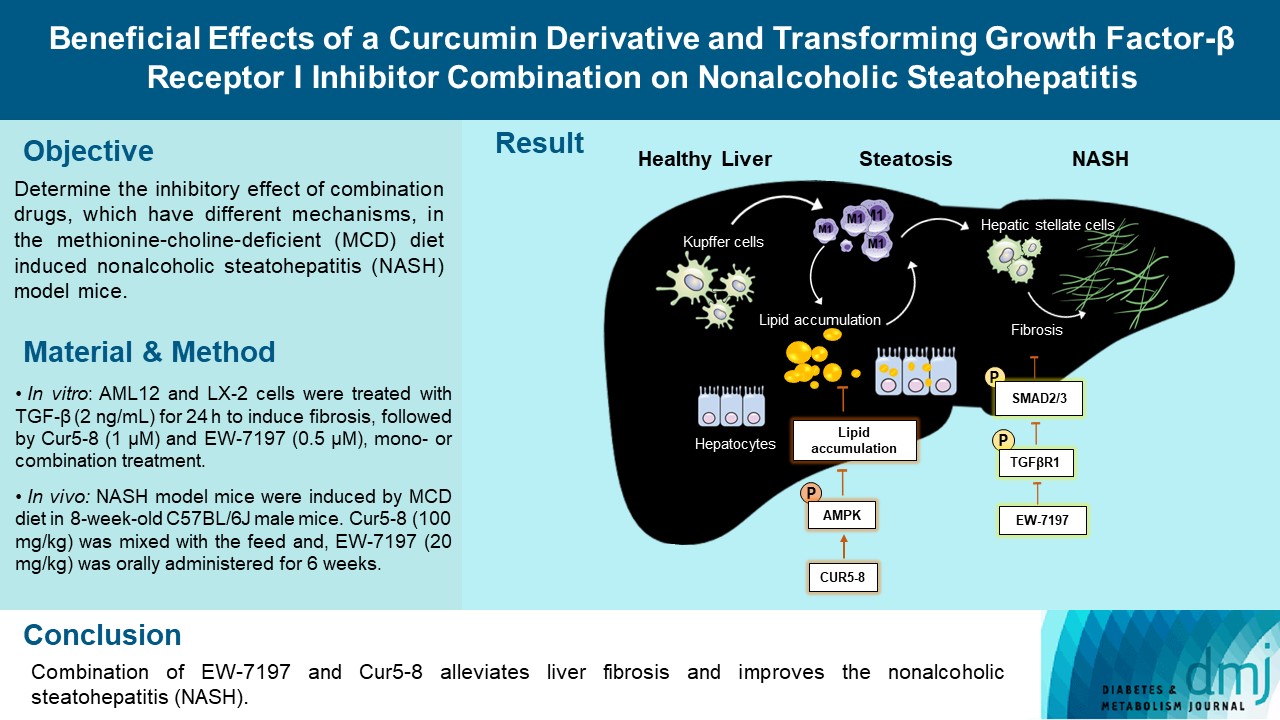
- Beneficial Effects of a Curcumin Derivative and Transforming Growth Factor-β Receptor I Inhibitor Combination on Nonalcoholic Steatohepatitis
- Kyung Bong Ha, Eun Soo Lee, Na Won Park, Su Ho Jo, Soyeon Shim, Dae-Kee Kim, Chan Mug Ahn, Choon Hee Chung
- Diabetes Metab J. 2023;47(4):500-513. Published online April 25, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0110
- 2,165 View
- 144 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Curcumin 2005-8 (Cur5-8), a derivative of curcumin, improves fatty liver disease via AMP-activated protein kinase activation and autophagy regulation. EW-7197 (vactosertib) is a small molecule inhibitor of transforming growth factor β (TGF-β) receptor I and may scavenge reactive oxygen species and ameliorate fibrosis through the SMAD2/3 canonical pathway. This study aimed to determine whether co-administering these two drugs having different mechanisms is beneficial.
Methods
Hepatocellular fibrosis was induced in mouse hepatocytes (alpha mouse liver 12 [AML12]) and human hepatic stellate cells (LX-2) using TGF-β (2 ng/mL). The cells were then treated with Cur5-8 (1 μM), EW-7197 (0.5 μM), or both. In animal experiments were also conducted during which, methionine-choline deficient diet, Cur5-8 (100 mg/kg), and EW-7197 (20 mg/kg) were administered orally to 8-week-old C57BL/6J mice for 6 weeks.
Results
TGF-β-induced cell morphological changes were improved by EW-7197, and lipid accumulation was restored on the administration of EW-7197 in combination with Cur5-8. In a nonalcoholic steatohepatitis (NASH)-induced mouse model, 6 weeks of EW-7197 and Cur5-8 co-administration alleviated liver fibrosis and improved the nonalcoholic fatty liver disease (NAFLD) activity score.
Conclusion
Co-administering Cur5-8 and EW-7197 to NASH-induced mice and fibrotic hepatocytes reduced liver fibrosis and steatohepatitis while maintaining the advantages of both drugs. This is the first study to show the effect of the drug combination against NASH and NAFLD. Similar effects in other animal models will confirm its potential as a new therapeutic agent.
- Drug/Regimen
- A Real-World Study of Long-Term Safety and Efficacy of Lobeglitazone in Korean Patients with Type 2 Diabetes Mellitus
- Bo-Yeon Kim, Hyuk-Sang Kwon, Suk Kyeong Kim, Jung-Hyun Noh, Cheol-Young Park, Hyeong-Kyu Park, Kee-Ho Song, Jong Chul Won, Jae Myung Yu, Mi Young Lee, Jae Hyuk Lee, Soo Lim, Sung Wan Chun, In-Kyung Jeong, Choon Hee Chung, Seung Jin Han, Hee-Seok Kim, Ju-Young Min, Sungrae Kim
- Diabetes Metab J. 2022;46(6):855-865. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0264
- 6,690 View
- 296 Download
- 6 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Thiazolidinediones (TZDs) have been associated with various safety concerns including weight gain, bladder cancer, and congestive heart failure (CHF). This study evaluated the efficacy and safety of lobeglitazone, a novel TZD in patients with type 2 diabetes mellitus (T2DM) in real practice.
Methods
In this non-interventional, multi-center, retrospective, and observational study conducted at 15 tertiary or secondary referral hospitals in Korea, a total of 2,228 patients with T2DM who received lobeglitazone 0.5 mg for more than 1 year were enrolled.
Results
Overall adverse events (AEs) occurred in 381 patients (17.10%) including edema in 1.97% (n=44). Cerebrovascular and cardiovascular diseases were identified in 0.81% (n=18) and 0.81% (n=18), respectively. One case of CHF was reported as an AE. Edema occurred in 1.97% (n=44) of patients. Hypoglycemia occurred in 2.47% (n=55) of patients. Fracture occurred in 1.17% (n=26) of all patients. Lobeglitazone significantly decreased HbA1c level, resulting in a mean treatment difference of -1.05%± 1.35% (P<0.001), and decreased total cholesterol, triglyceride, and low-density lipoprotein cholesterol. However, it increased high-density lipoprotein cholesterol, regardless of statin administration. The patients who received lobeglitazone 0.5 mg showed an apparent reduction in glycosylated hemoglobin (HbA1c) from baseline during the first 6 months of treatment. The HbA1c levels remained stable between months 6 and 42.
Conclusion
Lobeglitazone has long-term safety profile, good glycemic-lowering effect and long-term durability of glycemic control in real-world clinical settings. -
Citations
Citations to this article as recorded by- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
Deep Dutta, Saptarshi Bhattacharya, Manoj Kumar, Priyankar K. Datta, Ritin Mohindra, Meha Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102697. CrossRef - Efficacy and safety of lobeglitazone, a new Thiazolidinedione, as compared to the standard of care in type 2 diabetes mellitus: A systematic review and meta-analysis
Shashank R. Joshi, Saibal Das, Suja Xaviar, Shambo Samrat Samajdar, Indranil Saha, Sougata Sarkar, Shatavisa Mukherjee, Santanu Kumar Tripathi, Jyotirmoy Pal, Nandini Chatterjee
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102703. CrossRef - Will lobeglitazone rival pioglitazone? A systematic review and critical appraisal
Kalyan Kumar Gangopadhyay, Awadhesh Kumar Singh
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(4): 102747. CrossRef - Lobeglitazone
Reactions Weekly.2023; 1948(1): 262. CrossRef - Lobeglitazone, a novel thiazolidinedione, for secondary prevention in patients with ischemic stroke: a nationwide nested case-control study
Joonsang Yoo, Jimin Jeon, Minyoul Baik, Jinkwon Kim
Cardiovascular Diabetology.2023;[Epub] CrossRef - Lobeglitazone and Its Therapeutic Benefits: A Review
Balamurugan M, Sarumathy S, Robinson R
Cureus.2023;[Epub] CrossRef - Oldies but Goodies: Thiazolidinedione as an Insulin Sensitizer with Cardioprotection
Eun-Hee Cho
Diabetes & Metabolism Journal.2022; 46(6): 827. CrossRef
- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
- Clinical Diabetes & Therapeutics
- Effects of Lobeglitazone, a Novel Thiazolidinedione, on Bone Mineral Density in Patients with Type 2 Diabetes Mellitus over 52 Weeks
- Soo Lim, Kyoung Min Kim, Sin Gon Kim, Doo Man Kim, Jeong-Taek Woo, Choon Hee Chung, Kyung Soo Ko, Jeong Hyun Park, Yongsoo Park, Sang Jin Kim, Hak Chul Jang, Dong Seop Choi
- Diabetes Metab J. 2017;41(5):377-385. Published online October 24, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.5.377
- 4,258 View
- 42 Download
- 19 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aim of this multicenter, randomized, double-blind study was to examine the effect of lobeglitazone, a novel thiazolidinedione, on the changes in bone mineral density (BMD) in patients with type 2 diabetes mellitus.
Methods A 24-week, double-blinded phase was followed by a 28-week, open-label phase, in which the placebo group also started to receive lobeglitazone. A total of 170 patients aged 34 to 76 years were randomly assigned in a 2:1 ratio to receive lobeglitazone 0.5 mg or a matching placebo orally, once daily. BMD was assessed using dual-energy X-ray absorptiometry at week 24 and at the end of the study (week 52).
Results During the double-blinded phase, the femur neck BMD showed decreasing patterns in both groups, without statistical significance (−0.85%±0.36% and −0.78%±0.46% in the lobeglitazone and placebo groups, respectively). The treatment difference between the groups was 0.07%, which was also not statistically significant. Further, minimal, nonsignificant decreases were observed in both groups in the total hip BMD compared to values at baseline, and these differences also did not significantly differ between the groups. During the open-label phase, the BMD was further decreased, but not significantly, by −0.32% at the femur neck and by −0.60% at the total hip in the lobeglitazone group, and these changes did not significantly differ compared with the original placebo group switched to lobeglitazone.
Conclusion Our results indicate that treatment with lobeglitazone 0.5 mg over 52 weeks showed no detrimental effect on the BMD compared to the placebo.
-
Citations
Citations to this article as recorded by- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
Deep Dutta, Saptarshi Bhattacharya, Manoj Kumar, Priyankar K. Datta, Ritin Mohindra, Meha Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102697. CrossRef - Efficacy and safety of lobeglitazone, a new Thiazolidinedione, as compared to the standard of care in type 2 diabetes mellitus: A systematic review and meta-analysis
Shashank R. Joshi, Saibal Das, Suja Xaviar, Shambo Samrat Samajdar, Indranil Saha, Sougata Sarkar, Shatavisa Mukherjee, Santanu Kumar Tripathi, Jyotirmoy Pal, Nandini Chatterjee
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102703. CrossRef - The benefits of adipocyte metabolism in bone health and regeneration
Lisa-Marie Burkhardt, Christian H. Bucher, Julia Löffler, Charlotte Rinne, Georg N. Duda, Sven Geissler, Tim J. Schulz, Katharina Schmidt-Bleek
Frontiers in Cell and Developmental Biology.2023;[Epub] CrossRef - Will lobeglitazone rival pioglitazone? A systematic review and critical appraisal
Kalyan Kumar Gangopadhyay, Awadhesh Kumar Singh
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(4): 102747. CrossRef - Comparison of therapeutic efficacy and safety of sitagliptin, dapagliflozin, or lobeglitazone adjunct therapy in patients with type 2 diabetes mellitus inadequately controlled on sulfonylurea and metformin: Third agent study
Jun Hwa Hong, Jun Sung Moon, Kayeon Seong, Soo Lim
Diabetes Research and Clinical Practice.2023; 203: 110872. CrossRef - Bone Mineral Density Evaluation Among Type 2 Diabetic Patients in Rural Haryana, India: An Analytical Cross-Sectional Study
Nitish Khandelwal, Surbhi Rajauria, Siddhesh Pandurang Kanjalkar, Omkar Shivaji Chavanke, Sanjay Rai
Cureus.2023;[Epub] CrossRef - Lobeglitazone and Its Therapeutic Benefits: A Review
Balamurugan M, Sarumathy S, Robinson R
Cureus.2023;[Epub] CrossRef - A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - A Real-World Study of Long-Term Safety and Efficacy of Lobeglitazone in Korean Patients with Type 2 Diabetes Mellitus
Bo-Yeon Kim, Hyuk-Sang Kwon, Suk Kyeong Kim, Jung-Hyun Noh, Cheol-Young Park, Hyeong-Kyu Park, Kee-Ho Song, Jong Chul Won, Jae Myung Yu, Mi Young Lee, Jae Hyuk Lee, Soo Lim, Sung Wan Chun, In-Kyung Jeong, Choon Hee Chung, Seung Jin Han, Hee-Seok Kim, Ju-Y
Diabetes & Metabolism Journal.2022; 46(6): 855. CrossRef - Comparative Efficacy of Lobeglitazone Versus Pioglitazone on Albuminuria in Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes Therapy.2021; 12(1): 171. CrossRef - Lobeglitazone: A Novel Thiazolidinedione for the Management of Type 2 Diabetes Mellitus
Jaehyun Bae, Taegyun Park, Hyeyoung Kim, Minyoung Lee, Bong-Soo Cha
Diabetes & Metabolism Journal.2021; 45(3): 326. CrossRef - Effect of lobeglitazone on motor function in rat model of Parkinson’s disease with diabetes co-morbidity
Kambiz Hassanzadeh, Arman Rahimmi, Mohammad Raman Moloudi, Rita Maccarone, Massimo Corbo, Esmael Izadpanah, Marco Feligioni
Brain Research Bulletin.2021; 173: 184. CrossRef - Recent Perspective on Thiazolidinedione
Won Jun Kim
The Journal of Korean Diabetes.2021; 22(2): 97. CrossRef - Use of in vitro bone models to screen for altered bone metabolism, osteopathies, and fracture healing: challenges of complex models
Sabrina Ehnert, Helen Rinderknecht, Romina H. Aspera-Werz, Victor Häussling, Andreas K. Nussler
Archives of Toxicology.2020; 94(12): 3937. CrossRef - Update on: effects of anti-diabetic drugs on bone metabolism
Guillaume Mabilleau, Béatrice Bouvard
Expert Review of Endocrinology & Metabolism.2020; 15(6): 415. CrossRef - The use of metformin, insulin, sulphonylureas, and thiazolidinediones and the risk of fracture: Systematic review and meta‐analysis of observational studies
Khemayanto Hidayat, Xuan Du, Meng‐Jiao Wu, Bi‐Min Shi
Obesity Reviews.2019; 20(10): 1494. CrossRef - Diabetes pharmacotherapy and effects on the musculoskeletal system
Evangelia Kalaitzoglou, John L. Fowlkes, Iuliana Popescu, Kathryn M. Thrailkill
Diabetes/Metabolism Research and Reviews.2019;[Epub] CrossRef - Morin Exerts Anti‐Arthritic Effects by Attenuating Synovial Angiogenesis via Activation of Peroxisome Proliferator Activated Receptor‐γ
Mengfan Yue, Ni Zeng, Yufeng Xia, Zhifeng Wei, Yue Dai
Molecular Nutrition & Food Research.2018;[Epub] CrossRef - The effects of diabetes therapy on bone: A clinical perspective
Karim G. Kheniser, Carmen M. Polanco Santos, Sangeeta R. Kashyap
Journal of Diabetes and its Complications.2018; 32(7): 713. CrossRef - Changes in the Bone Mineral Density of Femur Neck and Total Hip Over a 52-Week Treatment with Lobeglitazone
Da Young Lee, Ji A Seo
Diabetes & Metabolism Journal.2017; 41(5): 374. CrossRef
- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
- Obesity and Metabolic Syndrome
- Relationship between Regional Body Fat Distribution and Diabetes Mellitus: 2008 to 2010 Korean National Health and Nutrition Examination Surveys
- Soo In Choi, Dawn Chung, Jung Soo Lim, Mi Young Lee, Jang Yel Shin, Choon Hee Chung, Ji Hye Huh
- Diabetes Metab J. 2017;41(1):51-59. Published online December 21, 2016
- DOI: https://doi.org/10.4093/dmj.2017.41.1.51
- 4,165 View
- 42 Download
- 35 Web of Science
- 36 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aim of this study was to investigate the association between regional body fat distribution, especially leg fat mass, and the prevalence of diabetes mellitus (DM) in adult populations.
Methods A total of 3,181 men and 3,827 postmenopausal women aged 50 years or older were analyzed based on Korea National Health and Nutrition Examination Surveys (2008 to 2010). Body compositions including muscle mass and regional fat mass were measured using dual-energy X-ray absorptiometry.
Results The odds ratios (ORs) for DM was higher with increasing truncal fat mass and arm fat mass, while it was lower with increasing leg fat mass. In a partial correlation analysis adjusted for age, leg fat mass was negatively associated with glycosylated hemoglobin in both sexes and fasting glucose in women. Leg fat mass was positively correlated with appendicular skeletal muscle mass and homeostasis model assessment of β cell. In addition, after adjusting for confounding factors, the OR for DM decreased gradually with increasing leg fat mass quartiles in both genders. When we subdivided the participants into four groups based on the median values of leg fat mass and leg muscle mass, higher leg fat mass significantly lowered the risk of DM even though they have smaller leg muscle mass in both genders (
P <0.001).Conclusion The relationship between fat mass and the prevalence of DM is different according to regional body fat distribution. Higher leg fat mass was associated with a lower risk of DM in Korean populations. Maintaining leg fat mass may be important in preventing impaired glucose tolerance.
-
Citations
Citations to this article as recorded by- Effects of chromium supplementation on body composition in patients with type 2 diabetes: A dose-response systematic review and meta-analysis of randomized controlled trials
Mahdi Vajdi, Mahsa khajeh, Ehsan Safaei, Seyedehelham Moeinolsadat, Samin Mousavi, Hooria Seyedhosseini-Ghaheh, Mahdieh Abbasalizad-Farhangi, Gholamreza Askari
Journal of Trace Elements in Medicine and Biology.2024; 81: 127338. CrossRef - Connections between body composition and dysregulation of islet α- and β-cells in type 2 diabetes
Jia-xi Miao, Jia-ping Xu, Rui Wang, Yu-xian Xu, Feng Xu, Chun-hua Wang, Chao Yu, Dong-mei Zhang, Jian-bin Su
Diabetology & Metabolic Syndrome.2024;[Epub] CrossRef - Anthropometric and DXA-derived measures of body composition in relation to pre-diabetes among adults
Anwar Mohammad, Ali H. Ziyab, Talal Mohammad
BMJ Open Diabetes Research & Care.2023; 11(5): e003412. CrossRef - A cohort study on the predictive capability of body composition for diabetes mellitus using machine learning
Mohammad Ali Nematollahi, Amir Askarinejad, Arefeh Asadollahi, Mehdi Bazrafshan, Shirin Sarejloo, Mana Moghadami, Sarvin Sasannia, Mojtaba Farjam, Reza Homayounfar, Babak Pezeshki, Mitra Amini, Mohamad Roshanzamir, Roohallah Alizadehsani, Hanieh Bazrafsha
Journal of Diabetes & Metabolic Disorders.2023;[Epub] CrossRef - Which is the best diet to reduce cardiometabolic risk: dietary counseling or home-delivered diet?
Feray Çağiran Yilmaz, Aysun Atilgan, Günay Saka
Food & Nutrition Research.2023;[Epub] CrossRef - Sedentary lifestyle and body composition in type 2 diabetes
Dan-dan Li, Yang Yang, Zi-yi Gao, Li-hua Zhao, Xue Yang, Feng Xu, Chao Yu, Xiu-lin Zhang, Xue-qin Wang, Li-hua Wang, Jian-bin Su
Diabetology & Metabolic Syndrome.2022;[Epub] CrossRef - Impaired Lung Function and Lung Cancer Incidence: A Nationwide Population-Based Cohort Study
Hye Seon Kang, Yong-Moon Park, Seung-Hyun Ko, Seung Hoon Kim, Shin Young Kim, Chi Hong Kim, Kyungdo Han, Sung Kyoung Kim
Journal of Clinical Medicine.2022; 11(4): 1077. CrossRef - Association between lung function and the risk of atrial fibrillation in a nationwide population cohort study
Su Nam Lee, Seung-Hyun Ko, Sung-Ho Her, Kyungdo Han, Donggyu Moon, Sung Kyoung Kim, Ki-Dong Yoo, Yu-Bae Ahn
Scientific Reports.2022;[Epub] CrossRef - Is imaging-based muscle quantity associated with risk of diabetes? A meta-analysis of cohort studies
Shanhu Qiu, Xue Cai, Yang Yuan, Bo Xie, Zilin Sun, Tongzhi Wu
Diabetes Research and Clinical Practice.2022; 189: 109939. CrossRef - Research Progress of Body Composition Changes in Type 2 Diabetes Patients
鹏霞 张
Advances in Clinical Medicine.2022; 12(08): 7181. CrossRef - Associations of eating speed with fat distribution and body shape vary in different age groups and obesity status
Saili Ni, Menghan Jia, Xuemiao Wang, Yun Hong, Xueyin Zhao, Liang Zhang, Yuan Ru, Fei Yang, Shankuan Zhu
Nutrition & Metabolism.2022;[Epub] CrossRef - Body composition, trabecular bone score and vertebral fractures in subjects with Klinefelter syndrome
W. Vena, F. Carrone, A. Delbarba, O. Akpojiyovbi, L. C. Pezzaioli, P. Facondo, C. Cappelli, L. Leonardi, L. Balzarini, D. Farina, A. Pizzocaro, A. G. Lania, G. Mazziotti, A. Ferlin
Journal of Endocrinological Investigation.2022; 46(2): 297. CrossRef - Genetically predicted body fat mass and distribution with diabetic kidney disease: A two-sample Mendelian randomization study
Min Wang, Xin Li, Hang Mei, Zhao-Hui Huang, Yue Liu, Yong-Hong Zhu, Tian-Kui Ma, Qiu-Ling Fan
Frontiers in Genetics.2022;[Epub] CrossRef - Screening for Prediabetes and Diabetes in Korean Nonpregnant Adults: A Position Statement of the Korean Diabetes Association, 2022
Kyung Ae Lee, Dae Jung Kim, Kyungdo Han, Suk Chon, Min Kyong Moon
Diabetes & Metabolism Journal.2022; 46(6): 819. CrossRef - Age- and Sex-Related Differential Associations between Body Composition and Diabetes Mellitus
Eun Roh, Soon Young Hwang, Jung A Kim, You-Bin Lee, So-hyeon Hong, Nam Hoon Kim, Ji A Seo, Sin Gon Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
Diabetes & Metabolism Journal.2021; 45(2): 183. CrossRef - Neck circumference and metabolic syndrome: A cross-sectional population-based study
Hooman Ebrahimi, Payam Mahmoudi, Farhad Zamani, Sedighe Moradi
Primary Care Diabetes.2021; 15(3): 582. CrossRef - Development of a clinical risk score for incident diabetes: A 10‐year prospective cohort study
Tae Jung Oh, Jae Hoon Moon, Sung Hee Choi, Young Min Cho, Kyong Soo Park, Nam H Cho, Hak Chul Jang
Journal of Diabetes Investigation.2021; 12(4): 610. CrossRef - The association of glucocorticoid receptor polymorphism with metabolic outcomes in menopausal women with adrenal incidentalomas
Sanja Ognjanović, Jadranka Antić, Tatjana Pekmezović, Bojana Popović, Tatjana Isailović, Ivana Božić Antić, Tamara Bogavac, Valentina Elezović Kovačević, Dušan Ilić, Milica Opalić, Djuro Macut
Maturitas.2021; 151: 15. CrossRef - Distinct opposing associations of upper and lower body fat depots with metabolic and cardiovascular disease risk markers
Mahasampath Gowri S, Belavendra Antonisamy, Finney S. Geethanjali, Nihal Thomas, Felix Jebasingh, Thomas V. Paul, Fredrik Karpe, Clive Osmond, Caroline H. D. Fall, Senthil K. Vasan
International Journal of Obesity.2021; 45(11): 2490. CrossRef - Body Roundness Index Is a Superior Obesity Index in Predicting Diabetes Risk Among Hypertensive Patients: A Prospective Cohort Study in China
Yingshan Liu, Xiaocong Liu, Haixia Guan, Shuting Zhang, Qibo Zhu, Xiaoying Fu, Hongmei Chen, Songtao Tang, Yingqing Feng, Jian Kuang
Frontiers in Cardiovascular Medicine.2021;[Epub] CrossRef - Subcutaneous adipose tissue distribution and serum lipid/lipoprotein in unmedicated postmenopausal women: A B-mode ultrasound study
Imaging.2021; 13(2): 119. CrossRef - The Leg Fat to Total Fat Ratio Is Associated with Lower Risks of Non-Alcoholic Fatty Liver Disease and Less Severe Hepatic Fibrosis: Results from Nationwide Surveys (KNHANES 2008–2011)
Hyun Min Kim, Yong-ho Lee
Endocrinology and Metabolism.2021; 36(6): 1232. CrossRef Optimal Cut-Offs of Body Mass Index and Waist Circumference to Identify Obesity in Chinese Type 2 Diabetic Patients
Qinying Zhao, Xiangjun Chen, Jinshan Wu, Lilin Gong, Jinbo Hu, Shumin Yang, Qifu Li, Zhihong Wang
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 1899. CrossRef- Weight Loss after 12 Weeks of Exercise and/or Nutritional Guidance Is Not Obligatory for Induced Changes in Local Fat/Lean Mass Indexes in Adults with Excess of Adiposity
Robinson Ramírez-Vélez, Mikel Izquierdo, Karem Castro-Astudillo, Carolina Medrano-Mena, Angela Liliana Monroy-Díaz, Rocío del Pilar Castellanos-Vega, Héctor Reynaldo Triana-Reina, María Correa-Rodríguez
Nutrients.2020; 12(8): 2231. CrossRef - VISCERAL FAT, PHYSICAL FITNESS AND BIOCHEMICAL MARKERS OF BRAZILIAN MILITARY PERSONNEL
Laércio Camilo Rodrigues, Marcos de Sá Rego Fortes, Marco Antônio Muniz Lippert, Samir Ezequiel Da Rosa, José Fernandes Filho
Revista Brasileira de Medicina do Esporte.2020; 26(1): 21. CrossRef - Comparison of 7-site skinfold measurement and dual-energy X-ray absorptiometry for estimating body fat percentage and regional adiposity in Taiwanese diabetic patients
Feng-Chih Kuo, Chieh-Hua Lu, Li-Wei Wu, Tung-Wei Kao, Sheng-Chiang Su, Jhih-Syuan Liu, Kuan-Chan Chen, Chia-Hao Chang, Chih-Chun Kuo, Chien-Hsing Lee, Chang-Hsun Hsieh, Mauro Lombardo
PLOS ONE.2020; 15(7): e0236323. CrossRef - Outcomes specific to patient sex after open ventral hernia repair
Kathryn A. Schlosser, Sean R. Maloney, Otto Thielan, Tanushree Prasad, Kent Kercher, Paul D. Colavita, B Todd Heniford, Vedra A. Augenstein
Surgery.2020; 167(3): 614. CrossRef Age-Related Changes in Body Composition and Bone Mineral Density and Their Relationship with the Duration of Diabetes and Glycaemic Control in Type 2 Diabetes
Ying Tang, Lilin Gong, Xiangjun Chen, Zhipeng Du, Jinbo Hu, Zhixin Xu, Jinshan Wu, Qifu Li, Zhihong Wang
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 4699. CrossRef- Lipodystrophy: A paradigm for understanding the consequences of "overloading" adipose tissue
Koini Lim, Afreen Haider, Claire Adams, Alison Sleigh, David Savage
Physiological Reviews.2020;[Epub] CrossRef - Premeal Consumption of a Protein-Enriched, Dietary Fiber-Fortified Bar Decreases Total Energy Intake in Healthy Individuals
Chang Ho Ahn, Jae Hyun Bae, Young Min Cho
Diabetes & Metabolism Journal.2019; 43(6): 879. CrossRef - Differences in dietary intakes, body compositions, and biochemical indices between metabolically healthy and metabolically abnormal obese Korean women
Eun Yeong Kang, Jung-Eun Yim
Nutrition Research and Practice.2019; 13(6): 488. CrossRef - The Association between Body Composition using Dual energy X-ray Absorptiometry and Type-2 Diabetes: A Systematic Review and Meta-Analysis of Observational studies
Preeti Gupta, Carla Lanca, Alfred T. L. Gan, Pauline Soh, Sahil Thakur, Yijin Tao, Neelam Kumari, Ryan E. K. Man, Eva K. Fenwick, Ecosse L. Lamoureux
Scientific Reports.2019;[Epub] CrossRef - Genes that make you fat, but keep you healthy
R. J. F. Loos, T. O. Kilpeläinen
Journal of Internal Medicine.2018; 284(5): 450. CrossRef - Overview of Epidemiology and Contribution of Obesity and Body Fat Distribution to Cardiovascular Disease: An Update
Marie-Eve Piché, Paul Poirier, Isabelle Lemieux, Jean-Pierre Després
Progress in Cardiovascular Diseases.2018; 61(2): 103. CrossRef - Relevance of human fat distribution on lipid and lipoprotein metabolism and cardiovascular disease risk
Marie-Eve Piché, Senthil K. Vasan, Leanne Hodson, Fredrik Karpe
Current Opinion in Lipidology.2018; 29(4): 285. CrossRef - Comparison of regional fat measurements by dual-energy X-ray absorptiometry and conventional anthropometry and their association with markers of diabetes and cardiovascular disease risk
S K Vasan, C Osmond, D Canoy, C Christodoulides, M J Neville, C Di Gravio, C H D Fall, F Karpe
International Journal of Obesity.2018; 42(4): 850. CrossRef
- Effects of chromium supplementation on body composition in patients with type 2 diabetes: A dose-response systematic review and meta-analysis of randomized controlled trials
- Diabetes Epidemics in Korea: Reappraise Nationwide Survey of Diabetes "Diabetes in Korea 2007"
- Ie Byung Park, Jaiyong Kim, Dae Jung Kim, Choon Hee Chung, Jee-Young Oh, Seok Won Park, Juneyoung Lee, Kyung Mook Choi, Kyung Wan Min, Jeong Hyun Park, Hyun Shik Son, Chul Woo Ahn, Hwayoung Kim, Sunhee Lee, Im Bong Lee, Injeoung Choi, Sei Hyun Baik
- Diabetes Metab J. 2013;37(4):233-239. Published online August 14, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.4.233
- 5,334 View
- 59 Download
- 62 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader There are many studies on the prevalence, clinical characteristics, and economic burden of diabetes across the past four decades in Korea. Nonetheless, there is a dearth of nationwide study regarding diabetes encompassing all age group. Eight years ago, the Committee on the Epidemiology of Diabetes Mellitus of Korean Diabetes Association collaborated with Health Insurance Review & Assessment Service to evaluate the status of diabetes care and characteristics in diabetic patients in Korea. In 2007, the collaborative task force team published a comprehensive survey titled "Diabetes in Korea 2007." In this review, we reappraise the diabetic epidemics from the joint report and suggest further studies that are needed to be investigated in the future.
-
Citations
Citations to this article as recorded by- Revisiting the Diabetes Crisis in Korea: Call for Urgent Action
Jun Sung Moon
The Journal of Korean Diabetes.2023; 24(1): 1. CrossRef - Risk assessment and classification for foot ulceration among patients with type 2 diabetes in South Korea
Eun Joo Lee, Ihn Sook Jeong, In Ju Kim, Young Hye Cho, Yun Jin Kim
International Journal of Nursing Practice.2022;[Epub] CrossRef - Using real-world data for supporting regulatory decision making: Comparison of cardiovascular and safety outcomes of an empagliflozin randomized clinical trial versus real-world data
Ha Young Jang, In-Wha Kim, Jung Mi Oh
Frontiers in Pharmacology.2022;[Epub] CrossRef - Differences in health behavior and nutrient intake status between diabetes-aware and unaware Korean adults based on the Korea national health and nutrition examination survey 2016–18 data: A cross-sectional study
Anshul Sharma, Chen Lulu, Kee-Ho Song, Hae-Jeung Lee
Frontiers in Public Health.2022;[Epub] CrossRef - Do statins benefit low-risk population for primary prevention of atherosclerotic cardiovascular disease: A retrospective cohort study
In Sun Ryou, Ju Young Kim, Hwa Yeon Park, Sohee Oh, Sehun Kim, Hwa Jung Kim
Frontiers in Medicine.2022;[Epub] CrossRef - Association between oseltamivir use and neuropsychiatric adverse events in influenza patients: a nationwide population-based cohort study
Hye-Rim Kang, Suk-Chan Jang, Ju-Young Shin
Expert Opinion on Drug Safety.2021; 20(2): 245. CrossRef - Effectiveness and safety of sodium‐glucose co‐transporter‐2 inhibitors compared with dipeptidyl peptidase‐4 inhibitors in older adults with type 2 diabetes: A nationwide population‐based study
Seung Jin Han, Kyoung Hwa Ha, Nami Lee, Dae Jung Kim
Diabetes, Obesity and Metabolism.2021; 23(3): 682. CrossRef - Cost-Effectiveness of Tiotropium in Elderly Patients with Severe Asthma Using Real-World Data
Sung-Hyun Hong, Jeong-Yeon Cho, Tae-Bum Kim, Eui-Kyung Lee, Sun-Hong Kwon, Ju-Young Shin
The Journal of Allergy and Clinical Immunology: In Practice.2021; 9(5): 1939. CrossRef - Dapagliflozin improves cardiovascular risk factors in Emirati patients with T2DM
Aml Mohamed Nada, Mariam Adel Younan
Therapeutic Advances in Endocrinology and Metabolism.2021; 12: 204201882199536. CrossRef - Association between socioeconomic position and diabetic foot ulcer outcomes: a population-based cohort study in South Korea
Jeong Hyun Ha, Heejin Jin, Ji-Ung Park
BMC Public Health.2021;[Epub] CrossRef - Etiology, diagnosis, complications, and treatments of diabetic foot
Dong-Kyo Seo
Journal of the Korean Medical Association.2021; 64(8): 523. CrossRef - Hospital admissions due to endocrine diseases in Korean male firefighters
Seunghoon Ryu, Yong-Jin Lee, Eun-Chul Jang, Soon-Chan Kwon, KiSeok Kim, Yeon-Soon Ahn, Young-Sun Min
Annals of Occupational and Environmental Medicine.2021;[Epub] CrossRef - Association between Frequency of Breakfast Consumption and Insulin Resistance Using Triglyceride-Glucose Index: A Cross-Sectional Study of the Korea National Health and Nutrition Examination Survey (2016–2018)
Hye Jin Joo, Gyu Ri Kim, Eun-Cheol Park, Sung-In Jang
International Journal of Environmental Research and Public Health.2020; 17(9): 3322. CrossRef - Review of Diabetic Foot Complication Assessment Tools Developed from 2007 to 2016
Yoonhee Lee, Youngshin Song
Journal of Korean Academy of Fundamentals of Nursing.2019; 26(4): 231. CrossRef - Associations between Breastfeeding and Type 2 Diabetes Mellitus and Glycemic Control in Parous Women: A Nationwide, Population-Based Study
Ga Eun Nam, Kyungdo Han, Do-Hoon Kim, Youn Huh, Byoungduck Han, Sung Jung Cho, Yong Gyu Park, Yong-Moon Park
Diabetes & Metabolism Journal.2019; 43(2): 236. CrossRef - Risk of osteoporosis in patients with chronic inflammatory neuropathy- a population-based cohort study
Seung Woo Kim, Eun Hwa Kim, Jinae Lee, Young-Chul Choi, Seung Min Kim, Ha Young Shin
Scientific Reports.2019;[Epub] CrossRef - Differences in the risk of mood disorders in patients with asthma-COPD overlap and in patients with COPD alone: a nationwide population-based retrospective cohort study in Korea
Hye-Rim Kang, Sung-Hyun Hong, So-Young Ha, Tae-Bum Kim, Eui-Kyung Lee
Respiratory Research.2019;[Epub] CrossRef - A Comparison of Leukotriene Receptor Antagonists to Low-Dose Inhaled Corticosteroids in the Elderly with Mild Asthma
Sung-Hyun Hong, Hye-Rim Kang, Jin Hyun Nam, Sun-Kyeong Park, Tae-Bum Kim, Eui-Kyung Lee
The Journal of Allergy and Clinical Immunology: In Practice.2019; 7(8): 2642. CrossRef - The Need to Improve the Quality of Diabetes Care in Korea
Seung Jin Han, Dae Jung Kim
Journal of Korean Medical Science.2019;[Epub] CrossRef - Fifty Years of Compassionate Care and Harmonious Collaboration of the Korean Diabetes Association: The 50th Anniversary of Korean Diabetes Association
Jong Chul Won, Eun-Jung Rhee, Hyung Joon Yoo
Diabetes & Metabolism Journal.2018; 42(6): 475. CrossRef - Depth and combined infection is important predictor of lower extremity amputations in hospitalized diabetic foot ulcer patients
Eun-Gyo Jeong, Sung Shim Cho, Sang-Hoon Lee, Kang-Min Lee, Seo-Kyung Woo, Yoongoo Kang, Jae-Seung Yun, Seon-Ah Cha, Yoon-Jung Kim, Yu-Bae Ahn, Seung-Hyun Ko, Jung-Min Lee
The Korean Journal of Internal Medicine.2018; 33(5): 952. CrossRef - Favorable glycemic response after pancreatoduodenectomy in both patients with pancreatic cancer and patients with non-pancreatic cancer
Seo Young Sohn, Eun Kyung Lee, Sung-Sik Han, You Jin Lee, Yul Hwangbo, Young Hwa Kang, Seung Duk Lee, Seong Hoon Kim, Sang Myung Woo, Woo Jin Lee, Eun Kyung Hong, Sang-Jae Park
Medicine.2018; 97(18): e0590. CrossRef - Clinical Importance of Diabetic Neuropathy
Tae Sun Park
The Journal of Korean Diabetes.2018; 19(3): 147. CrossRef - Women are less likely than men to achieve optimal glycemic control after 1 year of treatment: A multi-level analysis of a Korean primary care cohort
Seung-Ah Choe, Joo Yeong Kim, Young Sun Ro, Sung-Il Cho, Antonio Palazón-Bru
PLOS ONE.2018; 13(5): e0196719. CrossRef - Diagnosis and Management of Diabetic Foot
Chang Won Lee
The Journal of Korean Diabetes.2018; 19(3): 168. CrossRef - HbA1c Cutoff for Prediabetes and Diabetes Based on Oral Glucose Tolerance Test in Obese Children and Adolescents
Hyo-Kyoung Nam, Won Kyoung Cho, Jae Hyun Kim, Young-Jun Rhie, Sochung Chung, Kee-Hyoung Lee, Byung-Kyu Suh
Journal of Korean Medical Science.2018;[Epub] CrossRef - Diabetes Fact Sheet in Korea, 2016: An Appraisal of Current Status
Jong Chul Won, Jae Hyuk Lee, Jae Hyeon Kim, Eun Seok Kang, Kyu Chang Won, Dae Jung Kim, Moon-Kyu Lee
Diabetes & Metabolism Journal.2018; 42(5): 415. CrossRef - Risk factors of asthma exacerbation based on asthma severity: a nationwide population-based observational study in South Korea
Hye-Rim Kang, Hyun Jin Song, Jin Hyun Nam, Sung-Hyun Hong, So-Young Yang, SangEun Ju, Sang Won Lee, Tae-Bum Kim, Hye-Lin Kim, Eui-Kyung Lee
BMJ Open.2018; 8(3): e020825. CrossRef - Foot Care for Diabetic Patients
Hye Jung Cha
The Journal of Korean Diabetes.2018; 19(1): 41. CrossRef - Risk of new-onset diabetes among patients treated with statins according to hypertension and gender: Results from a nationwide health-screening cohort
Sang-Eun Lee, Ji Min Sung, In-Jeong Cho, Hyeon Chang Kim, Hyuk-Jae Chang, Lamberto Manzoli
PLOS ONE.2018; 13(4): e0195459. CrossRef - Treatment variation related to comorbidity and complications in type 2 diabetes
Yeon Young Cho, Sung-il Cho
Medicine.2018; 97(37): e12435. CrossRef - Efficacy of Body Weight Reduction on the SGLT2 Inhibitor in People with Type 2 Diabetes Mellitus
Hyun A Cho, Young Lee Jung, Yong Hoon Lee, Yu Chang Lee, Jung Eun Lee, Sol Jae Lee, Su Jin Jeong, Chong Hwa Kim
Journal of Obesity & Metabolic Syndrome.2017; 26(2): 107. CrossRef - Physician-Directed Diabetes Education without a Medication Change and Associated Patient Outcomes
Hun-Sung Kim, Hyunah Kim, Hae-Kyung Yang, Eun Young Lee, Yoo Jin Jeong, Tong Min Kim, So Jung Yang, Seo Yeon Baik, Seung-Hwan Lee, Jae Hyoung Cho, In Young Choi, Hyeon Woo Yim, Bong-Yun Cha
Diabetes & Metabolism Journal.2017; 41(3): 187. CrossRef - Current status of managing diabetes mellitus in Korea
Kyoung Hwa Ha, Dae Jung Kim
The Korean Journal of Internal Medicine.2016; 31(5): 845. CrossRef - 7th Asian PAD Workshop
Annals of Vascular Diseases.2016; 9(2): 135. CrossRef - Trends in Diabetes Incidence in the Last Decade Based on Korean National Health Insurance Claims Data
Sun Ok Song, Yong-ho Lee, Dong Wook Kim, Young Duk Song, Joo Young Nam, Kyoung Hye Park, Dae Jung Kim, Seok Won Park, Hyun Chul Lee, Byung-Wan Lee
Endocrinology and Metabolism.2016; 31(2): 292. CrossRef - Trends of antidiabetic drug use in adult type 2 diabetes in Korea in 2002–2013
Seung-Hyun Ko, Dae-Jung Kim, Jong-Heon Park, Cheol-Young Park, Chang Hee Jung, Hyuk-Sang Kwon, Joong-Yeol Park, Kee-Ho Song, Kyungdo Han, Ki-Up Lee, Kyung-Soo Ko
Medicine.2016; 95(27): e4018. CrossRef - Glycosylated Hemoglobin Threshold for Predicting Diabetes and Prediabetes from the Fifth Korea National Health and Nutrition Examination Survey
Sangmo Hong, Jun Goo Kang, Chul Sik Kim, Seong Jin Lee, Cheol-Young Park, Chang Beom Lee, Sung-Hee Ihm
Diabetes & Metabolism Journal.2016; 40(2): 167. CrossRef - Predictive Value of Glucose Parameters Obtained From Oral Glucose Tolerance Tests in Identifying Individuals at High Risk for the Development of Diabetes in Korean Population
Hae Kyung Yang, Hee-Sung Ha, Marie Rhee, Jin-Hee Lee, Yong-Moon Park, Hyuk-Sang Kwon, Hyeon-Woo Yim, Moo-Il Kang, Won-Chul Lee, Ho-Young Son, Seung-Hwan Lee, Kun-Ho Yoon
Medicine.2016; 95(10): e3053. CrossRef - Serum preadipocyte factor 1 concentrations and risk of developing diabetes: a nested case–control study
S. H. Lee, M. Rhee, H. K. Yang, H. S. Ha, J. H. Lee, H. S. Kwon, Y. M. Park, H. W. Yim, M. I. Kang, W. C. Lee, H. Y. Son, K. H. Yoon
Diabetic Medicine.2016; 33(5): 631. CrossRef - Is an Oral Glucose Tolerance Test Still Valid for Diagnosing Diabetes Mellitus?
Dong-Lim Kim, Sun-Doo Kim, Suk Kyeong Kim, Sooyoun Park, Kee-Ho Song
Diabetes & Metabolism Journal.2016; 40(2): 118. CrossRef - Fasting plasma glucose concentrations for specified HbA1c goals in Korean populations: data from the Fifth Korea National Health and Nutrition Examination Survey (KNHANES V-2, 2011)
Sangmo Hong, Jun Goo Kang, Chul Sik Kim, Seong Jin Lee, Chang Beom Lee, Sung-Hee Ihm
Diabetology & Metabolic Syndrome.2016;[Epub] CrossRef - Combined use of basal insulin analog and acarbose reduces postprandial glucose in patients with uncontrolled type 2 diabetes
Ji‐Hyun Kim, Ji‐Hyun Ahn, Soo‐Kyung Kim, Dae‐Ho Lee, Hye‐Soon Kim, Ho‐Sang Shon, Hyun‐Jeong Jeon, Tae‐Hwa Kim, Yong‐Wook Cho, Jae‐Taek Kim, Sung‐Min Han, Choon‐Hee Chung, Ohk‐Hyun Ryu, Jae‐Min Lee, Soon‐Hee Lee, Min‐Jeong Kwon, Tae‐kyun Kim, Il‐Seong Namg
Journal of Diabetes Investigation.2015; 6(2): 219. CrossRef - Anti-Oxidative and Anti-Diabetic Effects of Methanol Extracts from Medicinal Plants
Youn Ri Lee, Nara Yoon
Journal of the Korean Society of Food Science and Nutrition.2015; 44(5): 681. CrossRef - Associations Between the Continuity of Ambulatory Care of Adult Diabetes Patients in Korea and the Incidence of Macrovascular Complications
Young-Hoon Gong, Seok-Jun Yoon, Hyeyoung Seo, Dongwoo Kim
Journal of Preventive Medicine and Public Health.2015; 48(4): 188. CrossRef - Statin eligibility and cardiovascular risk burden assessed by coronary artery calcium score: Comparing the two guidelines in a large Korean cohort
Eun-Jung Rhee, Se Eun Park, Hyung Geun Oh, Cheol-Young Park, Ki-Won Oh, Sung-Woo Park, Ron Blankstein, Jorge Plutzky, Won-Young Lee
Atherosclerosis.2015; 240(1): 242. CrossRef - Evaluation of low-dose aspirin for primary prevention of ischemic stroke among patients with diabetes: a retrospective cohort study
Ye-Jee Kim, Nam-Kyong Choi, Mi-Sook Kim, Joongyub Lee, Yoosoo Chang, Jong-Mi Seong, Sun-Young Jung, Ju-Young Shin, Ji-Eun Park, Byung-Joo Park
Diabetology & Metabolic Syndrome.2015;[Epub] CrossRef - Health-Related Quality of Life in Coronary Heart Disease in Korea
Hyung Tak Lee, Jinho Shin, Young-Hyo Lim, Kyung Soo Kim, Soon Gil Kim, Jeong Hyun Kim, Heon Kil Lim
Angiology.2015; 66(4): 326. CrossRef - Seroepidemiology of varicella-zoster virus in Korean adolescents and adults using fluorescent antibody to membrane antigen test
S. B. HAN, K. R. KANG, D. H. HUH, H. C. LEE, J. H. KIM, J. H. KANG, S. H. MA
Epidemiology and Infection.2015; 143(8): 1643. CrossRef - Changing Clinical Characteristics according to Insulin Resistance and Insulin Secretion in Newly Diagnosed Type 2 Diabetic Patients in Korea
Jang Won Son, Cheol-Young Park, Sungrae Kim, Han-Kyu Lee, Yil-Seob Lee
Diabetes & Metabolism Journal.2015; 39(5): 387. CrossRef - Age- and Sex-Specific Relationships between Household Income, Education, and Diabetes Mellitus in Korean Adults: The Korea National Health and Nutrition Examination Survey, 2008-2010
So-Ra Kim, Kyungdo Han, Jin-Young Choi, Jennifer Ersek, Junxiu Liu, Sun-Jin Jo, Kang-Sook Lee, Hyeon Woo Yim, Won-Chul Lee, Yong Gyu Park, Seung-Hwan Lee, Yong-Moon Park, C. Mary Schooling
PLOS ONE.2015; 10(1): e0117034. CrossRef - Association between Diabetes Education Status and Clinical Outcomes of Patients with Diabetes Mellitus: Analysis of the Fifth Korea National Health and Nutrition Examination Survey (KNHANES V)
Jun Sung Kwon, Won Jun Kim, Yang Hee Han, Hyun Joong Kim, Sa Young Shin, Kyoo Ho Choi, Jae Hyuck Jun, Myoung Sook Shim, Jin Yeob Kim
The Journal of Korean Diabetes.2014; 15(4): 236. CrossRef - The Incidence and Prevalence of Diabetes Mellitus and Related Atherosclerotic Complications in Korea: A National Health Insurance Database Study
Bo Kyung Koo, Chang-Hoon Lee, Bo Ram Yang, Seung-sik Hwang, Nam-Kyong Choi, Mohammad Ebrahim Khamseh
PLoS ONE.2014; 9(10): e110650. CrossRef - Current Status of Glycemic Control of Patients with Diabetes in Korea: The Fifth Korea National Health and Nutrition Examination Survey
Ja Young Jeon, Dae Jung Kim, Seung-Hyun Ko, Hyuk-Sang Kwon, Soo Lim, Sung Hee Choi, Chul Sik Kim, Jee Hyun An, Nan Hee Kim, Jong Chul Won, Jae Hyeon Kim, Bong-Yun Cha, Kee-Ho Song
Diabetes & Metabolism Journal.2014; 38(3): 197. CrossRef - Strong correlation between glycaemic variability and total glucose exposure in type 2 diabetes is limited to subjects with satisfactory glycaemic control
S. Suh, J.Y. Joung, S.M. Jin, M.Y. Kim, J.C. Bae, H.D. Park, M.S. Lee, M.K. Lee, J.H. Kim
Diabetes & Metabolism.2014; 40(4): 272. CrossRef - Current Status of Diabetic Peripheral Neuropathy in Korea: Report of a Hospital-Based Study of Type 2 Diabetic Patients in Korea by the Diabetic Neuropathy Study Group of the Korean Diabetes Association
Jong Chul Won, Sang Soo Kim, Kyung Soo Ko, Bong-Yun Cha
Diabetes & Metabolism Journal.2014; 38(1): 25. CrossRef - Impact of Age at First Childbirth on Glucose Tolerance Status in Postmenopausal Women: The 2008–2011 Korean National Health and Nutrition Examination Survey
Jin Hwa Kim, Yun Jung, Sang Yong Kim, Hak Yeon Bae
Diabetes Care.2014; 37(3): 671. CrossRef - Predicting the Development of Diabetes Using the Product of Triglycerides and Glucose: The Chungju Metabolic Disease Cohort (CMC) Study
Seung-Hwan Lee, Hyuk-Sang Kwon, Yong-Moon Park, Hee-Sung Ha, Seung Hee Jeong, Hae Kyung Yang, Jin-Hee Lee, Hyeon-Woo Yim, Moo-Il Kang, Won-Chul Lee, Ho-Young Son, Kun-Ho Yoon, Maria Eugenia Saez
PLoS ONE.2014; 9(2): e90430. CrossRef - Relationship between socioeconomic status and type 2 diabetes: results from Korea National Health and Nutrition Examination Survey (KNHANES) 2010-2012
J. Hwang, C. Shon
BMJ Open.2014; 4(8): e005710. CrossRef - Diabetes Mellitus and Osteoporosis
Kyoung Min Kim
The Journal of Korean Diabetes.2013; 14(4): 186. CrossRef - Study on the Correlation between the Nutrient Intakes and Clinical Indices of Type 2 Diabetes Patients
Ji-Young Kwon, Hae-Yun Chung
The Korean Journal of Food And Nutrition.2013; 26(4): 909. CrossRef - Role of Sarcopenia in Diabetes Mellitus
Sang Youl Rhee
The Journal of Korean Diabetes.2013; 14(4): 178. CrossRef
- Revisiting the Diabetes Crisis in Korea: Call for Urgent Action
- Role of HbA1c in the Screening of Diabetes Mellitus in a Korean Rural Community
- Jae Hyun Kim, Gun Woo Kim, Mi Young Lee, Jang Yel Shin, Young Goo Shin, Sang Baek Koh, Choon Hee Chung
- Diabetes Metab J. 2012;36(1):37-42. Published online February 17, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.1.37
- 3,732 View
- 33 Download
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Recently, the measurement of glycated hemoglobin (HbA1c) was recommended as an alternative to fasting plasma glucose or oral glucose tolerance tests for diagnosing diabetes mellitus (DM). In this study, we analyzed HbA1c levels for diabetes mellitus screening in a Korean rural population.
Methods We analyzed data from 10,111 subjects from a Korean Rural Genomic Cohort study and generated a receiver operating characteristic curve to determine an appropriate HbA1c cutoff value for diabetes.
Results The mean age of the subjects was 56.3±8.1 years. Fasting plasma glucose and 2-hour plasma glucose after 75 g oral glucose tolerance tests were 97.5±25.6 and 138.3±67.1 mg/dL, respectively. The mean HbA1c level of the subjects was 5.7±0.9%. There were 8,809 non-DM patients (87.1%) and 1,302 DM patients (12.9%). A positive relationship between HbA1c and plasma glucose levels and between HbA1c and 2-hour plasma glucose levels after oral glucose tolerance tests was found in a scatter plot of the data. Using Youden's index, the proper cutoff level of HbA1c for diabetes mellitus screening was 5.95% (sensitivity, 77%; specificity, 89.4%).
Conclusion Our results suggest that the optimal HbA1c level for DM screening is 5.95%.
-
Citations
Citations to this article as recorded by- Hyperinsulinemia: an early biomarker of metabolic dysfunction
Rama A. Vaidya, Sharvari Desai, Panchali Moitra, Sheryl Salis, Shubhada Agashe, Rekha Battalwar, Anushree Mehta, Jagmeet Madan, Soumik Kalita, Shobha A. Udipi, Ashok B. Vaidya
Frontiers in Clinical Diabetes and Healthcare.2023;[Epub] CrossRef - A Novel Earwax Method to Measure Acute and Chronic Glucose Levels
Andrés Herane-Vives, Susana Espinoza, Rodrigo Sandoval, Lorena Ortega, Luis Alameda, Allan H. Young, Danilo Arnone, Alexander Hayes, Jan Benöhr
Diagnostics.2020; 10(12): 1069. CrossRef - Risk Factors for Underdiagnosis of Diabetes Based on the Korean National Health and Nutrition Examination Survey 2013-2015
Deulle Min, Eunhee Cho
Asia Pacific Journal of Public Health.2019; 31(5): 404. CrossRef - Recent advances of medical journals in Korea and and further development strategies: Is it possible for them to publish Nobel Prize-winning research?
Sun Huh
Journal of the Korean Medical Association.2018; 61(9): 524. CrossRef - The clinical value of HbA1c in combination with FPG in the early screening of the elderly with type 2 diabetes
Lihua Liu, Wenqing Chen, Minghua Dong, Lixia Jiang, Wei Qiu, Jian Li, Xiaoting Luo, Zhengchun Huang, Qin Wu, Qinfeng Wu, Shuiqin Chen, Lu Ou-Yang, Shumei Li, J.Q. Cheng, H.L. Moffitt, I. Kim, Z.T. Chi, J. Zhang
BIO Web of Conferences.2017; 8: 01030. CrossRef - The Cutoff Value of HbA1c in Predicting Diabetes and Impaired Fasting Glucose
Seyoung Kwon, Youngak Na
The Korean Journal of Clinical Laboratory Science.2017; 49(2): 114. CrossRef - Performance of HbA1c for the prediction of diabetes in a rural community in Korea
B. M. Song, H. C. Kim, J. Y. Lee, J.‐M. Lee, D. J. Kim, Y.‐H. Lee, I. Suh
Diabetic Medicine.2015; 32(12): 1602. CrossRef - The Relationship between BMI and Glycated Albumin to Glycated Hemoglobin (GA/A1c) Ratio According to Glucose Tolerance Status
Ji Hye Huh, Kwang Joon Kim, Byung-Wan Lee, Dong Wook Kim, Eun Seok Kang, Bong Soo Cha, Hyun Chul Lee, Marta Letizia Hribal
PLoS ONE.2014; 9(2): e89478. CrossRef - Additional perspectives on chronic kidney disease of unknown aetiology (CKDu) in Sri Lanka – lessons learned from the WHO CKDu population prevalence study
Jennifer Hoponick Redmon, Myles F Elledge, Donna S Womack, Rajitha Wickremashinghe, Kamani P Wanigasuriya, Roshini J Peiris-John, Joseph Lunyera, Kristin Smith, James H Raymer, Keith E Levine
BMC Nephrology.2014;[Epub] CrossRef - Diagnostic Efficiency of Hemoglobin A1c for Newly Diagnosed Diabetes and Prediabetes in Community-Based Chinese Adults Aged 40 Years or Older
Kai Liang, Yu Sun, Wen-juan Li, Xiu-ping Zhang, Cheng-qiao Li, Wei-fang Yang, Ze-qiang Ma, Ai-xia Ma, Hui-zhen Zheng, Jun Song, Peng Lin, Xin-guo Hou, Li Chen
Diabetes Technology & Therapeutics.2014; 16(12): 853. CrossRef - Diagnostic accuracy of HbA1c in diabetes between Eastern and Western
Shuang Yan, Siying Liu, Yashuang Zhao, Wencui Zhang, Xiaohui Sun, Jianing Li, Fuli Jiang, Jiaming Ju, Ning Lang, Yingqi Zhang, Weiyu Zhou, Qiang Li
European Journal of Clinical Investigation.2013; 43(7): 716. CrossRef
- Hyperinsulinemia: an early biomarker of metabolic dysfunction
- Effects of Spironolactone and Losartan on Diabetic Nephropathy in a Type 2 Diabetic Rat Model
- Mi Young Lee, Myoung Sook Shim, Bo Hwan Kim, Soon Won Hong, Ran Choi, Eun Young Lee, Soo Min Nam, Gun Woo Kim, Jang Yel Shin, Young Goo Shin, Choon Hee Chung
- Diabetes Metab J. 2011;35(2):130-137. Published online April 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.2.130
- 3,697 View
- 64 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background While there is an evidence that the anti-inflammatory properties of spironolactone can attenuate proteinuria in type 2 diabetes, its effects on vascular endothelial growth factor (VEGF) expression in diabetic nephropathy have not been clearly defined. In this study, we examined the effects of spironolactone, losartan, and a combination of these two drugs on albuminuria, renal VEGF expression, and inflammatory and oxidative stress markers in a type 2 diabetic rat model.
Methods Thirty-three Otsuka-Long-Evans-Tokushima-Fatty (OLETF) rats were divided into four groups and treated with different medication regimens from weeks 25 to 50; OLETF diabetic controls (
n =5), spironolactone-treated (n =10), losartan-treated (n =9), and combination of spironolactone- and losartan-treated (n =9).Results At week 50, the albumin-to-creatinine ratio was significantly decreased in the losartan and combination groups compared to the control OLETF group. No decrease was detected in the spironolactone group. There was a significant reduction in renal VEGF, transforming growth factor (TGF)-β, and type IV collagen mRNA levels in the spironolactone- and combination regimen-treated groups. Twenty-four hour urine monocyte chemotactic protein-1 levels were comparable in all four groups but did show a decreasing trend in the losartan and combination regimen groups. Twenty-four hour urine malondialdehyde levels were significantly decreased in the spironolactone- and combination regimen-treated groups.
Conclusion These results suggest that losartan alone and a combined regimen of spironolactone and losartan could ameliorate albuninuria by reducing renal VEGF expression. Also, simultaneous treatment with spironolactone and losartan may have protective effects against diabetic nephropathy by decreasing TGF-β and type IV collagen expression and by reducing oxidative stress in a type 2 diabetic rat model.
-
Citations
Citations to this article as recorded by- Tetrahydrocurcumin Add‐On therapy to losartan in a rat model of diabetic nephropathy decreases blood pressure and markers of kidney injury
Mahyar Khazaeli, Ane C. F. Nunes, Yitong Zhao, Mahziar Khazaali, John Prudente, Nosratola D. Vaziri, Bhupinder Singh, Wei Ling Lau
Pharmacology Research & Perspectives.2023;[Epub] CrossRef - Type 2 Diabetes Mellitus: Pathogenic Features and Experimental Models in Rodents
Inessa G. Gvazava, M. V. Karimova, A. V. Vasiliev, E. A. Vorotelyak
Acta Naturae.2022; 14(3): 57. CrossRef - Role of mineralocorticoid receptor antagonists in kidney diseases
Vishal Patel, Amit Joharapurkar, Mukul Jain
Drug Development Research.2021; 82(3): 341. CrossRef - Multi-strain probiotic supplement attenuates streptozotocin-induced type-2 diabetes by reducing inflammation and β-cell death in rats
Pei-Shan Hsieh, Hsieh-Hsun Ho, Shu Ping Tsao, Shih-Hung Hsieh, Wen-Yang Lin, Jui-Fen Chen, Yi-Wei Kuo, Shin-Yu Tsai, Hui-Yu Huang, Michael W. Greene
PLOS ONE.2021; 16(6): e0251646. CrossRef - Ocular surface complications in diabetes: The interrelationship between insulin and enkephalin
Indira Purushothaman, Ian S. Zagon, Joseph W. Sassani, Patricia J. McLaughlin
Biochemical Pharmacology.2021; 192: 114712. CrossRef - Mineralocorticoid Receptor Antagonists in Diabetic Kidney Disease
Daiji Kawanami, Yuichi Takashi, Yoshimi Muta, Naoki Oda, Dai Nagata, Hiroyuki Takahashi, Makito Tanabe
Frontiers in Pharmacology.2021;[Epub] CrossRef - Effects of single and dual RAAS blockade therapy on progressive kidney disease transition to CKD in rats
Devesh Aggarwal, Gaaminepreet Singh
Naunyn-Schmiedeberg's Archives of Pharmacology.2020; 393(4): 615. CrossRef - Bioactive Agent Discovery from the Natural Compounds for the Treatment of Type 2 Diabetes Rat Model
Shih-Chun Yang, Ching-Yun Hsu, Wei-Ling Chou, Jia-You Fang, Shih-Yi Chuang
Molecules.2020; 25(23): 5713. CrossRef - Losartan improves renal function and pathology in obese ZSF-1 rats
Zhi Su, Deborah Widomski, Arthur Nikkel, Laura Leys, Marian Namovic, Diana Donnelly-Roberts, Murali Gopalakrishnan, Steve McGaraughty
Journal of Basic and Clinical Physiology and Pharmacology.2018; 29(3): 281. CrossRef - Analyzing polymeric nanofibrous scaffold performances in diabetic animal models for translational chronic wound healing research
Nowsheen Goonoo, Archana Bhaw-Luximon
Nanotechnology Reviews.2017; 6(6): 583. CrossRef - Stimulatory effect of insulin on renal proximal tubule sodium transport is preserved in type 2 diabetes with nephropathy
Motonobu Nakamura, Nobuhiko Satoh, Masashi Suzuki, Haruki Kume, Yukio Homma, George Seki, Shoko Horita
Biochemical and Biophysical Research Communications.2015; 461(1): 154. CrossRef - Combination therapy with spironolactone and candesartan protects against streptozotocin-induced diabetic nephropathy in rats
Amal Hofni, Mohamed A. El-Moselhy, Ashraf Taye, Mohamed M. Khalifa
European Journal of Pharmacology.2014; 744: 173. CrossRef - Renal Protective Role of Xiexin Decoction with Multiple Active Ingredients Involves Inhibition of Inflammation through Downregulation of the Nuclear Factor-κB Pathway in Diabetic Rats
Jia-sheng Wu, Rong Shi, Jie Zhong, Xiong Lu, Bing-liang Ma, Tian-ming Wang, Bin Zan, Yue-ming Ma, Neng-neng Cheng, Fu-rong Qiu
Evidence-Based Complementary and Alternative Medicine.2013; 2013: 1. CrossRef - The use of animal models in diabetes research
Aileen JF King
British Journal of Pharmacology.2012; 166(3): 877. CrossRef - Effect of Eplerenone, a Selective Aldosterone Blocker, on the Development of Diabetic Nephropathy in Type 2 Diabetic Rats
Jae Hee Ahn, Ho Cheol Hong, Myong Jin Cho, Yoon Jung Kim, Hae Yoon Choi, Chai Ryoung Eun, Sae Jeong Yang, Hye Jin Yoo, Hee Young Kim, Ji A Seo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Dong Seop Choi, Nan Hee Kim
Diabetes & Metabolism Journal.2012; 36(2): 128. CrossRef
- Tetrahydrocurcumin Add‐On therapy to losartan in a rat model of diabetic nephropathy decreases blood pressure and markers of kidney injury
- Relationship Between Metabolic Syndrome and Risk of Chronic Complications in Koreans with Type 2 Diabetes.
- Hye Soo Chung, Ji A Seo, Sin Gon Kim, Nan Hee Kim, Doo Man Kim, Choon Hee Chung, Dong seop Choi
- Korean Diabetes J. 2009;33(5):392-400. Published online October 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.5.392
- 2,032 View
- 26 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
We examined the relationships between components of metabolic syndrome at the time of diagnosis of type 2 diabetes, and the development of chronic complications in Korean patients with type 2 diabetes. METHODS: The medical records of patients with type 2 diabetes who had undergone treatment for at least five years prior were collected from 10 general hospitals in Korea. Among a total of 1,418 patients reviewed for possible inclusion in this study, 603 patients were selected, and the occurrence of complications among these patients was evaluated. RESULTS: Among the 603 patients (male, 253; female, 350), 154 males (60.8%) and 266 females (76.0%) were diagnosed with metabolic syndrome at the time of initial diagnosis of type 2 diabetes. The incidence of chronic complications (average follow-up 15.2 +/- 4.9 years) included 60 cases of coronary artery disease (CAD), 57 cases of cerebrovascular accident (CVA), 268 cases of diabetic retinopathy (DR), 254 cases of diabetic nephropathy (DN), and 238 cases of diabetic peripheral neuropathy (DPN). As compared to patients without metabolic syndrome, the adjusted relative risks (95% CI) of incidental diabetic complications in patients with metabolic syndrome were 3.28 (1.40~7.71) for CAD, 2.04 (0.86~4.82) for CVA, 1.53 (1.10~2.14) for DR, 1.90 (1.29~2.80) for DN, and 1.51, (1.06~2.14) for DPN. With the addition of just one constituent of metabolic syndrome, the relative risk of developing CAD, CVD, DR, DN, and DPN increased by 2.08 (95% CI, 1.27~3.40), 1.16 (0.80~1.66), 1.09 (0.93~1.26), 1.29 (1.06~1.57) and 1.06 (0.87~1.26), respectively. CONCLUSION: Metabolic syndrome in Korean patients with type 2 diabetes increases the risk of developing both macrovascular and microvascular complications. -
Citations
Citations to this article as recorded by- COVID-19 pandemic: Effects of national lockdown on the state of health of patients with type 2 diabetes mellitus in a Moroccan population
Hamid Farhane, Majida Motrane, Fatima-Ezzahra Anaibar, Aïcha Motrane, Said Nassor Abeid, Nourdin Harich
Primary Care Diabetes.2021; 15(5): 772. CrossRef - Profil clinique du syndrome métabolique et facteurs associés à sa présence au cours du diabète de type 2 à Ouagadougou (Burkina Faso)
O. Guira, H. Tiéno, Y. Sagna, P. Mayodé, D. Yanogo, L. Zoungrana, C.-G. Kyélem, M.-T. Yaméogo, J.-Y. Drabo
Médecine des Maladies Métaboliques.2016; 10(1): 70. CrossRef - The Relationship between Metabolic Syndrome and Quality of Life in Korean Adult Women
Hyung-Su Park, Jong Park
The Journal of the Korea institute of electronic communication sciences.2013; 8(4): 639. CrossRef - Diabetes Risk Analysis Model with Personalized Food Intake Preference
So-Hye Jeon, Nam-Hyun Kim
Journal of the Korea Academia-Industrial cooperation Society.2013; 14(11): 5771. CrossRef - Comorbidity Study on Type 2 Diabetes Mellitus Using Data Mining
Hye Soon Kim, A Mi Shin, Mi Kyung Kim, Yoon Nyun Kim
The Korean Journal of Internal Medicine.2012; 27(2): 197. CrossRef - Cardio-Metabolic Features of Type 2 Diabetes Subjects Discordant in the Diagnosis of Metabolic Syndrome
Sa Rah Lee, Ying Han, Ja Won Kim, Ja Young Park, Ji Min Kim, Sunghwan Suh, Mi-Kyoung Park, Hye-Jeong Lee, Duk Kyu Kim
Diabetes & Metabolism Journal.2012; 36(5): 357. CrossRef
- COVID-19 pandemic: Effects of national lockdown on the state of health of patients with type 2 diabetes mellitus in a Moroccan population
- A Nationwide Survey about the Current Status of Glycemic Control and Complications in Diabetic Patients in 2006: The Committee of the Korean Diabetes Association on the Epidemiology of Diabetes Mellitus.
- Soo Lim, Dae Jung Kim, In Kyung Jeong, Hyun Shik Son, Choon Hee Chung, Gwanpyo Koh, Dae Ho Lee, Kyu Chang Won, Jeong Hyun Park, Tae Sun Park, Jihyun Ahn, Jaetaek Kim, Keun Gyu Park, Seung Hyun Ko, Yu Bae Ahn, Inkyu Lee
- Korean Diabetes J. 2009;33(1):48-57. Published online February 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.1.48
- 2,769 View
- 55 Download
- 43 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The Committee of the Korean Diabetes Association on the Epidemiology of Diabetes Mellitus performed a nationwide survey about the current status of glycemic control and diabetic complications in 2006. METHODS: The current study included 5,652 diabetic patients recruited from the rosters of endocrinology clinics of 13 tertiary hospitals in Korea. Age, gender, height, weight, waist circumference and blood pressure were investigated by standard method. Fasting and postprandial 2 hour glucose, glycosylated hemoglobin (HbA1c), lipid profiles, fasting insulin and c-peptide levels were measured. Microvascular (microalbuminuria, retinopathy and neuropathy) and macrovascular (coronary artery disease [CAD], cerebrovascular disease [CVD] and peripheral artery disease [PAD]) complications were reviewed in their medical records. RESULTS: Mean age of total subjects was 58.7 (+/- 11.6) years and duration of diabetes was 8.8 (0~50) years. Mean fasting and postprandial 2 hour glucose levels were 145.9 +/- 55.0 and 208.0 +/- 84.4 mg/dL, respectively. Their mean HbA1c was 7.9 +/- 1.9%: the percentage of patients within target goal of glycemic control (< 7% of HbA1c) was 36.7%. In this study, 30.3%, 38.3% and 44.6% of patients was found to have microalbuminuria, retinopathy and nephropathy, respectively. Prevalence of CAD, CVD and PAD was 8.7%, 6.7% and 3.0%, respectively. Diabetic complications were closely related with age, duration of diabetes and glycemic control, and this relationship was stronger in microvascular complications than macrovascular ones. CONCLUSION: Only about one third of patients with diabetes was found to reach target glycemic control in tertiary hospitals of Korea. More tight control is needed to reduce deleterious complications of diabetes in Korea. -
Citations
Citations to this article as recorded by- Risk of Diabetic Complications in Type 2 Diabetes Patients with Dementia: A Population-Based Study Using National Health Insurance Claims Data
Eun Sik Jeong, Ah-Young Kim, Hye-Young Kang
Drug Targets and Therapeutics.2023; 2(1): 49. CrossRef - Prevalence of thyroid disorders in type 2 diabetic patients – A 1-year cross-sectional study
RikitaRamesh Mudhol, ShivakumarVeeranna Turamari, RekhaRamesh Mudhol, B Srinivas
BLDE University Journal of Health Sciences.2022; 7(1): 56. CrossRef - Associations of fasting glucose and glycated hemoglobin with vitamin D levels according to diabetes mellitus status in Korean adults
Yerin Hwang, Jiyoung Jang, Myung-Hee Shin
Epidemiology and Health.2022; 44: e2022025. CrossRef - Atherectomy in Peripheral Artery Disease: Current and Future
Yohan Kwon, Jinoo Kim, Je-Hwan Won, Seong Ho Kim, Jeong-Eun Kim, Sung-Joon Park
Journal of the Korean Society of Radiology.2021; 82(3): 551. CrossRef - Diabetic Retinopathy and Related Clinical Practice for People with Diabetes in Korea: A 10-Year Trend Analysis
Yoo-Ri Chung, Kyoung Hwa Ha, Kihwang Lee, Dae Jung Kim
Diabetes & Metabolism Journal.2020; 44(6): 928. CrossRef - Current status of treatment of type 2 diabetes mellitus in Ningbo, China
Tianmeng Yang, Rongjiong Zheng, Qingmei Chen, Yushan Mao
Journal of Clinical Laboratory Analysis.2019;[Epub] CrossRef - Recently Uncontrolled Glycemia in Diabetic Patients Is Associated with the Severity of Intracranial Atherosclerosis
Nari Choi, Jeong-Yoon Lee, Jun-Sang Sunwoo, Hakjae Roh, Moo-Young Ahn, Sung-Tae Park, Kyung Bok Lee
Journal of Stroke and Cerebrovascular Diseases.2017; 26(11): 2615. CrossRef - The effect of educational program based on the precede-proceed model on improving self-care behaviors in a semi-urban population with type 2 diabetes referred to health centers of Bavi, Iran
Neda Barasheh, Ghodratollah Shakerinejad, Sedigheh Nouhjah, Mohammad Hossein Haghighizadeh
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2017; 11: S759. CrossRef - Increased prevalence of albuminuria in individuals with higher range of impaired fasting glucose: the 2011 Korea National Health and Nutrition Examination Survey
Jong Chul Won, Jae Won Hong, Jung Min Kim, Tae Nyun Kim, Jung Hyun Noh, Kyung Soo Ko, Byoung Doo Rhee, Dong-Jun Kim
Journal of Diabetes and its Complications.2015; 29(1): 50. CrossRef - Assessment of glycemic control in patients with type 2 diabetes mellitus treated with metformin–sulfonylurea combination: Results of a multicenter, cross‐sectional, observational study in Korea
Sin Gon Kim, Jong Ryeal Hahm, Duk Kyu Kim, Sung Rae Cho, Dong Seop Choi
Journal of Diabetes Investigation.2015; 6(3): 317. CrossRef - Current Status of Management in Type 2 Diabetes Mellitus at General Hospitals in South Korea
Jin-Hee Jung, Jung-Hwa Lee, Jin-Won Noh, Jeong-Eun Park, Hee-Sook Kim, Joo-Wha Yoo, Bok-Rye Song, Jeong-rim Lee, Myeong-Hee Hong, Hyang-Mi Jang, Young Na, Hyun-Joo Lee, Jeong-Mi Lee, Yang-Gyo Kang, Sun-Young Kim, Kang-Hee Sim
Diabetes & Metabolism Journal.2015; 39(4): 307. CrossRef - Kidney injury molecule-1 (Kim-1): an early biomarker for nephropathy in type II diabetic patients
Nahla E. El-Ashmawy, Enas A. El-Zamarany, Naglaa F. Khedr, Abeer I. Abd El-Fattah, Shereen A. Eltoukhy
International Journal of Diabetes in Developing Countries.2015; 35(S3): 431. CrossRef - The Effect of the Experience of Diabetes Education on Knowledge, Self-Care Behavior and Glycosylated Hemoglobin in Type 2 Diabetic Patients
Seung Hei Moon, Young Whee Lee, Ok-Kyung Ham, Soo-Hyun Kim
The Journal of Korean Academic Society of Nursing Education.2014; 20(1): 81. CrossRef - Clinical Characteristics of Diabetic Patients Transferred to Korean Referral Hospitals
Min Young Oh, Sang Soo Kim, In Joo Kim, In Kyu Lee, Hong Sun Baek, Hyoung Woo Lee, Min Young Chung
Diabetes & Metabolism Journal.2014; 38(5): 388. CrossRef - Current Status of Prescription in Type 2 Diabetic Patients from General Hospitals in Busan
Ji Hye Suk, Chang Won Lee, Sung Pyo Son, Min Cheol Kim, Jun Hyeob Ahn, Kwang Jae Lee, Ja Young Park, Sun Hye Shin, Min Jeong Kwon, Sang Soo Kim, Bo Hyun Kim, Soon Hee Lee, Jeong Hyun Park, In Joo Kim
Diabetes & Metabolism Journal.2014; 38(3): 230. CrossRef - The Influence of Admission Hypoglycemia on Clinical Outcomes in Acute Myocardial Infarction Patients with Diabetes Mellitus
Eun Jung Kim, Myung Ho Jeong, In Seok Jeong, Sang Gi Oh, Sang Hyung Kim, Young keun Ahn, Ju Han Kim, Young Jo Kim, Shung Chull Chae, Taek Jong Hong, In Whan Seong, Jei Keon Chae, Chong Jin Kim, Myeong Chan Cho, Ki Bae Seung, Hyo Soo Kim
Korean Journal of Medicine.2014; 87(5): 565. CrossRef - Duration of diabetes and effectiveness of insulin in the management of insulin-naïve Korean patients uncontrolled on oral antidiabetic drugs: a sub-analysis of the MOdaliTy of Insulin treatment eValuation (MOTIV) registry results
Sang Soo Kim, In Joo Kim, Yong Ki Kim, Kun Ho Yoon, Ho Young Son, Sung Woo Park, Yeon Ah Sung, Hong Sun Baek, Kyoung Soo Ha
Acta Diabetologica.2014; 51(4): 655. CrossRef - Is the Indicator Magnifying Window for Insulin Pens Helpful for Elderly Diabetic Patients?
Ju Hee Lee, Eun Shil Hong, Jung Hun Ohn, Young Min Cho
Diabetes & Metabolism Journal.2013; 37(2): 149. CrossRef - Prevalence of and Factors Associated with Albuminuria in the Korean Adult Population: The 2011 Korea National Health and Nutrition Examination Survey
Jong Chul Won, Yun Jeong Lee, Jung Min Kim, Sang Youb Han, Jung Hyun Noh, Kyung Soo Ko, Byoung Doo Rhee, Dong-Jun Kim, Harald Mischak
PLoS ONE.2013; 8(12): e83273. CrossRef - The Epidemiology of Diabetic Nephropathy
Jin Hwa Kim
The Journal of Korean Diabetes.2013; 14(1): 11. CrossRef - The Relationship between Neuropathic Pain and Glycemic Control, Self Management in Type II Diabetes Mellitus Patients
Yeong-Mi Seo, Won-Hee Choi
Journal of the Korea Academia-Industrial cooperation Society.2013; 14(4): 1774. CrossRef - Efficacy and Safety of Biphasic Insulin Aspart 30/70 in Type 2 Diabetes Suboptimally Controlled on Oral Antidiabetic Therapy in Korea: A Multicenter, Open-Label, Single-Arm Study
Kee-Ho Song, Jung Min Kim, Jung-Hyun Noh, Yongsoo Park, Hyun-Shik Son, Kyong Wan Min, Kyung Soo Ko
Diabetes & Metabolism Journal.2013; 37(2): 117. CrossRef - Comorbidity Study on Type 2 Diabetes Mellitus Using Data Mining
Hye Soon Kim, A Mi Shin, Mi Kyung Kim, Yoon Nyun Kim
The Korean Journal of Internal Medicine.2012; 27(2): 197. CrossRef - Low ankle-brachial index is an independent predictor of poor functional outcome in acute cerebral infarction
Jinkwon Kim, Dong Hyun Lee, Myoung-Jin Cha, Tae-Jin Song, Ji Hye Park, Hye Sun Lee, Chung Mo Nam, Hyo Suk Nam, Young Dae Kim, Ji Hoe Heo
Atherosclerosis.2012; 224(1): 113. CrossRef - Glucose, Blood Pressure, and Lipid Control in Korean Adults with Diagnosed Diabetes
Sun-Joo Boo
Korean Journal of Adult Nursing.2012; 24(4): 406. CrossRef - Diabetic Peripheral Neuropathy in Type 2 Diabetes Mellitus in Korea
Seung-Hyun Ko, Bong-Yun Cha
Diabetes & Metabolism Journal.2012; 36(1): 6. CrossRef - The Association of Self-Reported Coronary Heart Disease with Diabetes Duration in Korea
Hye Mi Kang, Yun Jeong Lee, Dong-Jun Kim
Diabetes & Metabolism Journal.2012; 36(5): 350. CrossRef - Response: The Prevalence of Peripheral Arterial Disease in Korean Patients with Type 2 Diabetes Mellitus Attending a University Hospital (Diabetes Metab J 2011;35:543-50)
Ji Hee Yu, Ki-Up Lee
Diabetes & Metabolism Journal.2012; 36(1): 77. CrossRef - Reduction in glycated albumin can predict change in HbA1c: comparison of oral hypoglycaemic agent and insulin treatments
H. K. Won, K. J. Kim, B.‐W. Lee, E. S. Kang, B. S. Cha, H. C. Lee
Diabetic Medicine.2012; 29(1): 74. CrossRef - Management of Blood Pressure in Patients with Type 2 Diabetes Mellitus: A Nationwide Survey in Korean
Mi Hae Seo, Woo Je Lee, Cheol Young Park, Sung Rae Kim, Joong Yeol Park, Kun-Ho Yoon, Moon Kyu Lee, Sung Woo Park
Diabetes & Metabolism Journal.2011; 35(4): 348. CrossRef - Accuracy Evaluation of the Alternative Site Blood Glucose Test Using Error Grid
Kyung-Soon Park, Eun-Jong Cha
Journal of Biomedical Engineering Research.2011; 32(1): 25. CrossRef - Glycated albumin is a useful glycation index for monitoring fluctuating and poorly controlled type 2 diabetic patients
Eun Young Lee, Byung-Wan Lee, Daham Kim, Yong-ho Lee, Kwang Joon Kim, Eun Seok Kang, Bong-Soo Cha, Eun Jig Lee, Hyun Chul Lee
Acta Diabetologica.2011; 48(2): 167. CrossRef - Group Classification on Management Behavior of Diabetic Mellitus
Sung-Hong Kang, Soon-Ho Choi
Journal of the Korea Academia-Industrial cooperation Society.2011; 12(2): 765. CrossRef - Predictive Clinical Parameters for the Therapeutic Efficacy of Sitagliptin in Korean Type 2 Diabetes Mellitus
Soon Ae Kim, Woo Ho Shim, Eun Hae Lee, Young Mi Lee, Sun Hee Beom, Eun Sook Kim, Jeong Seon Yoo, Ji Sun Nam, Min Ho Cho, Jong Suk Park, Chul Woo Ahn, Kyung Rae Kim
Diabetes & Metabolism Journal.2011; 35(2): 159. CrossRef - Epidemiology of Micro- and Macrovascular Complications of Type 2 Diabetes in Korea
Jung Hee Kim, Dae Jung Kim, Hak Chul Jang, Sung Hee Choi
Diabetes & Metabolism Journal.2011; 35(6): 571. CrossRef - Increasing Trend in the Number of Severe Hypoglycemia Patients in Korea
Jin Taek Kim, Tae Jung Oh, Ye An Lee, Jun Ho Bae, Hyo Jeong Kim, Hye Seung Jung, Young Min Cho, Kyong Soo Park, Soo Lim, Hak Chul Jang, Hong Kyu Lee
Diabetes & Metabolism Journal.2011; 35(2): 166. CrossRef - Prevalence and Associated Factors of Diabetic Retinopathy in Rural Korea: The Chungju Metabolic Disease Cohort Study
Ji-Hyun Kim, Hyuk-Sang Kwon, Yong-Moon Park, Jin-Hee Lee, Man-Soo Kim, Kun-Ho Yoon, Won Chul Lee, Bong-Yun Cha, Ho-Young Son
Journal of Korean Medical Science.2011; 26(8): 1068. CrossRef - The Prevalence of Peripheral Arterial Disease in Korean Patients with Type 2 Diabetes Mellitus Attending a University Hospital
Ji Hee Yu, Jenie Yoonoo Hwang, Mi-Seon Shin, Chang Hee Jung, Eun Hee Kim, Sang Ah Lee, Eun Hee Koh, Woo Je Lee, Min-Seon Kim, Joong-Yeol Park, Ki-Up Lee
Diabetes & Metabolism Journal.2011; 35(5): 543. CrossRef - Prevalence, Awareness, and Control of Hypertension among Diabetic Koreans
Hyun Hee Chung, Kyu Chang Won
Diabetes & Metabolism Journal.2011; 35(4): 337. CrossRef - Factors Influencing Physical Activity Behavior among Iranian Women with Type 2 Diabetes Using the Extended Theory of Reasoned Action
Alireza Didarloo, Davoud Shojaeizadeh, Hassan Eftekhar Ardebili, Shamsaddin Niknami, Ebrahim Hajizadeh, Mohammad Alizadeh
Diabetes & Metabolism Journal.2011; 35(5): 513. CrossRef - Factors that Affect Medication Adherence in Elderly Patients with Diabetes Mellitus
Kyung-Ae Park, Jung-Guk Kim, Bo-Wan Kim, Sin Kam, Keon-Yeop Kim, Sung-Woo Ha, Sung-Taek Hyun
Korean Diabetes Journal.2010; 34(1): 55. CrossRef - The Effects of Tailored Diabetes Education on Blood Glucose Control and Self-Care
Kyung Sun Hyun, Kwang Mi Kim, Sook Hee Jang
Journal of Korean Academy of Nursing.2009; 39(5): 720. CrossRef - Epidemiologic Characteristics of Diabetes Mellitus in Korea: Current Status of Diabetic Patients Using Korean Health Insurance Database
Ie Byung Park, Sei Hyun Baik
Korean Diabetes Journal.2009; 33(5): 357. CrossRef
- Risk of Diabetic Complications in Type 2 Diabetes Patients with Dementia: A Population-Based Study Using National Health Insurance Claims Data
- Prevalence of the Metabolic Syndrome in Type 2 Diabetic Patients.
- Tae Ho Kim, Dae Jung Kim, Soo Lim, In Kyung Jeong, Hyun Shik Son, Choon Hee Chung, Gwanpyo Koh, Dae Ho Lee, Kyu Chang Won, Jeong Hyun Park, Tae Sun Park, Jihyun Ahn, Jaetaek Kim, Keun Gyu Park, Seung Hyun Ko, Yu Bae Ahn, Inkyu Lee
- Korean Diabetes J. 2009;33(1):40-47. Published online February 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.1.40
- 2,379 View
- 27 Download
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The aim of this study was to analyze the prevalence of metabolic syndrome in Korean type 2 diabetic patients. METHODS: A total of 4,240 diabetic patients (male 2,033, female 2,207; mean age 58.7 +/- 11.3 years; DM duration 8.9 +/- 7.6 years) were selected from the data of endocrine clinics of 13 university hospitals in 2006. Metabolic syndrome was defined using the criteria of the American Heart Association/National Heart Lung and Blood Institute and the criteria of waist circumference from the Korean Society for the Study of Obesity. RESULTS: The prevalence of metabolic syndrome was 77.9% (76.7% of males, 78.9% of females). The average number of the components of metabolic syndrome was 2.4 +/- 1.1. Abdominal obesity was seen in 56.8% of the patients, hypertriglyceridemia in 42.0%, low HDL cholesterol in 65.1%, and high blood pressure in 74.9%. Abdominal obesity and high blood pressure were much more prevalent among females than males, and low HDL cholesterol was much more prevalent among males than females. The prevalence of metabolic syndrome was not different according to the duration of diabetes. Metabolic syndrome was strongly related with obesity (odds ratio, 6.3) and increased age (odds ratio in the over 70 group, 3.4). CONCLUSION: The prevalence of metabolic syndrome was 77.9% in Korean type 2 diabetic patients. Its prevalence was greater in obese patients and in those over 40 years of age. -
Citations
Citations to this article as recorded by- A Novel Clinical Predictor of Metabolic Syndrome: Vascular Risk Age
Abdulrahman Naser, Didar Elif Akgün, Rengin Çetin Güvenç, Samet Sayılan, Özgen Şafak
Bagcilar Medical Bulletin.2023; 9(1): 1. CrossRef - Risk of Carotid Atherosclerosis in Subjects with Prediabetes Overlapping Metabolic Syndrome
Seol A Jang, Kyoung Min Kim, Seok Won Park, Chul Sik Kim
Metabolic Syndrome and Related Disorders.2022; 20(10): 599. CrossRef - Metabolic Age, an Index Based on Basal Metabolic Rate, Can Predict Individuals That are High Risk of Developing Metabolic Syndrome
Sarahi Vásquez-Alvarez, Sergio K. Bustamante-Villagomez, Gabriela Vazquez-Marroquin, Leonardo M. Porchia, Ricardo Pérez-Fuentes, Enrique Torres-Rasgado, Oscar Herrera-Fomperosa, Ivette Montes-Arana, M. Elba Gonzalez-Mejia
High Blood Pressure & Cardiovascular Prevention.2021; 28(3): 263. CrossRef - Metabolic syndrome among type 2 diabetic patients in Sub-Saharan African countries: A systematic review and meta-analysis
Wondimeneh Shibabaw Shiferaw, Tadesse Yirga Akalu, Mihretie Gedefaw, Denis Anthony, Ayelign Mengesha Kassie, Worku Misganaw Kebede, Henok Mulugeta, Getenet Dessie, Yared Asmare Aynalem
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2020; 14(5): 1403. CrossRef - Optimal Waist Circumference Cutoff Value Based on Insulin Resistance and Visceral Obesity in Koreans with Type 2 Diabetes
Jung Soo Lim, Young Ju Choi, Soo-Kyung Kim, Byoung Wook Huh, Eun Jig Lee, Kap Bum Huh
Diabetes & Metabolism Journal.2015; 39(3): 253. CrossRef - The Relations between Diabetic Dietary Compliance, Dietary Intake, and Physical Activity and the Prevalence of Metabolic Syndrome (MS) in Type 2 Diabetic Patients
Dong Eun Kim, Seung Hee Hong, Ji-Myung Kim
Korean Journal of Community Nutrition.2015; 20(5): 351. CrossRef - The Comparison between Periodontal Health Status and the Findings of Hypertension and Diabetes Disease of some Workers
In-Young Ku, Seon-Jeong Moon, Kyung-Hwan Ka, Myeong-Seon Lee
The Korean Journal of Health Service Management.2013; 7(2): 81. CrossRef - The Relationship between Factors of Metabolic Syndrome in Korean Adult Males and the Parents' Family History of Diabetes
Hyung-Su Park, Jin-Gyu Jeong, Jin-Ho Yu
The Journal of the Korea institute of electronic communication sciences.2013; 8(5): 779. CrossRef - Associations of serum fetuin-A levels with insulin resistance and vascular complications in patients with type 2 diabetes
Chan-Hee Jung, Bo-Yeon Kim, Chul-Hee Kim, Sung-Koo Kang, Sang-Hee Jung, Ji-Oh Mok
Diabetes and Vascular Disease Research.2013; 10(5): 459. CrossRef - Cardio-Metabolic Features of Type 2 Diabetes Subjects Discordant in the Diagnosis of Metabolic Syndrome
Sa Rah Lee, Ying Han, Ja Won Kim, Ja Young Park, Ji Min Kim, Sunghwan Suh, Mi-Kyoung Park, Hye-Jeong Lee, Duk Kyu Kim
Diabetes & Metabolism Journal.2012; 36(5): 357. CrossRef - Comorbidity Study on Type 2 Diabetes Mellitus Using Data Mining
Hye Soon Kim, A Mi Shin, Mi Kyung Kim, Yoon Nyun Kim
The Korean Journal of Internal Medicine.2012; 27(2): 197. CrossRef - Therapeutic Target Achievement in Type 2 Diabetic Patients after Hyperglycemia, Hypertension, Dyslipidemia Management
Ah Young Kang, Su Kyung Park, So Young Park, Hye Jeong Lee, Ying Han, Sa Ra Lee, Sung Hwan Suh, Duk Kyu Kim, Mi Kyoung Park
Diabetes & Metabolism Journal.2011; 35(3): 264. CrossRef - The Correlations between Extremity Circumferences with Total and Regional Amounts of Skeletal Muscle and Muscle Strength in Obese Women with Type 2 Diabetes
Hwi Ryun Kwon, Kyung Ah Han, Hee Jung Ahn, Jae Hyuk Lee, Gang Seo Park, Kyung Wan Min
Diabetes & Metabolism Journal.2011; 35(4): 374. CrossRef
- A Novel Clinical Predictor of Metabolic Syndrome: Vascular Risk Age
- Relationship between Menopausal Status and Metabolic Syndrome Components in Korean Women.
- Jang Hyun Koh, Mi Young Lee, Soo Min Nam, Joong Kyung Sung, Pil Moon Jung, Jin Kyu Noh, Jang Yel Shin, Young Goo Shin, Choon Hee Chung
- Korean Diabetes J. 2008;32(3):243-251. Published online June 1, 2008
- DOI: https://doi.org/10.4093/kdj.2008.32.3.243
- 2,334 View
- 35 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Postmenopausal status is associated with a 60% increased risk for metabolic syndrome. It is thought to be associated with decreased estrogens and increased abdominal obesity in postmenopausal women with metabolic syndrome. The purpose of this study was to investigate the association between metabolic syndrome components and menopausal status. METHODS: A total of 1,926 women were studied and divided into three groups according to their menstrual stage (premenopausal, perimenopausal or postmenopausal). The presence of metabolic syndrome was assessed using the National Cholesterol Education Program's (NCEP) Adult Treatment Panel III criteria. RESULTS: The prevalence of metabolic syndrome was 7.1% in premenopause, 9.8% in perimenopause, and 24.2% in postmenopause. The strong correlation was noted between the metabolic syndrome score and waist circumference in postmenopause (r = 0.56, P < 0.01) and perimenopause (r = 0.60, P < 0.01). Along the menopausal transition, the risk of metabolic syndrome increased with high triglyceride after the age-adjusted (odds ratio (OR) 1.517 [95% confidence interval (CI) 1.014~2.269] in perimenopausal women and OR 1.573 [95% CI 1.025~2.414] in postmenopausal women). In addition, the prevalence of metabolic syndromeincreased in accordance with elevated alanine aminotransferase (ALT) and gamma-glutamyl transpeptidase (GGT) levels. CONCLUSION: Triglyceride and waist circumference were important metabolic syndrome components, though ALT and GGT may also be related for predicting metabolic syndrome during the transition to menopause. -
Citations
Citations to this article as recorded by- Interaction between major dietary patterns and cardiorespiratory fitness on metabolic syndrome in Iranian adults: a cross-sectional study
Hossein Shahinfar, Mahtab Ghanbari, Yahya Jalilpiran, Nastaran Payande, Mahshid Shahavandi, Nadia Babaei, Kurosh Djafarian, Cain C. C. Clark, Sakineh Shab-Bidar
Nutrition Journal.2021;[Epub] CrossRef - The Effects of Wild Ginseng Complex Pharmacopuncture Combined with Hyperthermia on Abdominal Obesity in Post-Menopause Women: Case Report
Jeong-Eun Yoo
Journal of Korean Medicine for Obesity Research.2016; 16(2): 133. CrossRef - Factors associated with metabolic syndrome in climacteric women of southern Brazil
A. D. Rodrigues, H. Theodoro, K. G. Mendes, V. M. Paniz, D. de Lorenzi, M. T. Anselmo Olinto
Climacteric.2012; 16(1): 96. CrossRef - Effects of Web-based Health Education on Blood Glucose and Blood Pressure Improvement in Postmenopausal Women with Impaired Fasting Blood Glucose
Jeong-Ah Oh, Hee-Seung Kim, Min-Jeong Park, Hye-Sun Shim
Journal of Korean Academy of Nursing.2011; 41(5): 724. CrossRef - Prevalence of Metabolic Syndrome and Related Risk Factors of Elderly Residents in Andong Rural Area 2. Based on the Biochemical Measurements and Nutrient Intakes
Hye-Sang Lee, Chong-Suk Kwon
Journal of the Korean Society of Food Science and Nutrition.2010; 39(10): 1459. CrossRef - The Association between Serum GGT Concentration and Diabetic Peripheral Polyneuropathy in Type 2 Diabetic Patients
Ho Chan Cho
Korean Diabetes Journal.2010; 34(2): 111. CrossRef - Prevalence of Metabolic Syndrome and Related Risk Factors of Elderly Residents in Andong Rural Area 1. Based on the Anthropometric Measurements and Health Behaviors
Hye-Sang Lee, Chong-Suk Kwon
Journal of the Korean Society of Food Science and Nutrition.2010; 39(4): 511. CrossRef
- Interaction between major dietary patterns and cardiorespiratory fitness on metabolic syndrome in Iranian adults: a cross-sectional study
- The Role of Glomerular Podocytes in Diabetic Nephropathy.
- Eun Young Lee, Choon Hee Chung
- Korean Diabetes J. 2007;31(6):451-454. Published online November 1, 2007
- DOI: https://doi.org/10.4093/jkda.2007.31.6.451
- 2,141 View
- 19 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Diabetic nephropathy is the most common cause of end-stage renal disease and accounts for significant morbidity and mortality among individuals with diabetes mellitus. Therefore, the clarification of the pathogenesis of diabetic nephropathy is an urgent issue. Podocytes cover the outer layer of the glomerulus and maintain its integrity so that fluid and toxins exit in urine, but cells and important proteins are kept in the blood stream. Diabetes mellitus alters this structure, it becomes scarred and then the ability of the kidney to clear toxins is lost. Recent evidence shows that early in diabetes the podocyte number is reduced, areas of the glomerular basement membrane are denuded, and podocyte number predicts long-term urinary albumin excretion in the patients with diabetes and microalbuminuria. These results suggest that podocytes play a critical role in the early stage of diabetic nephropathy. It is the purpose of this article to review the pathogenetic role of podocytes in diabetic nephropathy.
-
Citations
Citations to this article as recorded by- Inhibition of dipeptidyl peptidase-4 (DPP4), antioxidant, antiglycation and anti-inflammatory effect of Ferulic acid against streptozotocin toxicity mediate nephropathy in diabetic rats
Maryam A. AL-Ghamdi, Said S. Moselhy
Environmental Science and Pollution Research.2022; 30(12): 33942. CrossRef - Study of Antiglycation, Hypoglycemic, and Nephroprotective Activities of the Green Dwarf Variety Coconut Water (Cocos nucifera L.) in Alloxan-Induced Diabetic Rats
Isabella F.D. Pinto, Railmara P. Silva, Adriano de B. Chaves Filho, Lucas S. Dantas, Vanderson S. Bispo, Isaac A. Matos, Felipe A.M. Otsuka, Aline C. Santos, Humberto Reis Matos
Journal of Medicinal Food.2015; 18(7): 802. CrossRef - Effects of ferulic acid on diabetic nephropathy in a rat model of type 2 diabetes
Ran Choi, Bo Hwan Kim, Jarinyaporn Naowaboot, Mi Young Lee, Mi Ri Hyun, Eun Ju Cho, Eun Soo Lee, Eun Young Lee, Young Chul Yang, Choon Hee Chung
Experimental and Molecular Medicine.2011; 43(12): 676. CrossRef
- Inhibition of dipeptidyl peptidase-4 (DPP4), antioxidant, antiglycation and anti-inflammatory effect of Ferulic acid against streptozotocin toxicity mediate nephropathy in diabetic rats
- Current Status of Diabetes Management in Korea Using National Health Insurance Database.
- Seok Won Park, Dae Jung Kim, Kyung Wan Min, Sei Hyun Baik, Kyung Mook Choi, Ie Byung Park, Jeong Hyun Park, Hyun Shik Son, Chul Woo Ahn, Jee Young Oh, Juneyoung Lee, Choon Hee Chung, Jaiyong Kim, Hwayoung Kim
- Korean Diabetes J. 2007;31(4):362-367. Published online July 1, 2007
- DOI: https://doi.org/10.4093/jkda.2007.31.4.362
- 2,837 View
- 33 Download
- 31 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The prevalence of diabetes is steadily increasing in Korea. The increase in number of people with diabetes would ultimately result in premature death, poor quality of life, and increasing economic burden. However, in our country, researches regarding on the quality of diabetes management are lacking. This study was conducted in 2005 using National Health Insurance Database to know the current status of diabetes management in Korea. METHODS: We have randomly selected 3,902 subjects out of 2,503,754 subjects who had claims with diagnosis of diabetes between January 2003 to December 2003 by using two staged cluster sampling method. Field survey with review of medical records and telephone survey was conducted with standardized record forms developed by Korean Diabetes Association; Task Force Team For Basic Statistical Study of Korean Diabetes Mellitus. RESULTS: The age of diabetic subjects was 58.1 +/- 12.6 years and the duration of diabetes was 6.2 +/- 5.5 years. Hypertension was present in 54% of diabetic subjects. Among those with hypertension, 59% were controlled with blood pressure below 140/90 mmHg, but only 19% were controlled with blood pressure below 130/80 mmHg. Hyperlipidemia was present in 29% of diabetic subjects. Only 38% of those with hyperlipidemia were controlled with LDL-cholesterol below 100 mg/dL. For glycemic control, only 40% of diabetic subjects achieved the goal of HbA1c less than 7%, which was suggested by ADA. CONCLUSION: We found that only 20~40% of diabetic subjects in Korea achieved the management goal for glucose, blood pressure, and lipids. It seems urgent to develop a quality management program for diabetes subjects in Korea. -
Citations
Citations to this article as recorded by- Developing a nomogram for predicting depression in diabetic patients after COVID-19 using machine learning
Haewon Byeon
Frontiers in Public Health.2023;[Epub] CrossRef - Factors Influencing the Utilization of Diabetes Complication Tests Under the COVID-19 Pandemic: Machine Learning Approach
Haewon Byeon
Frontiers in Endocrinology.2022;[Epub] CrossRef - Influences of Patient Activation on Diabetes Self-Care Activities and Diabetes-Specific Distress
Sookyung Choi, Su Hyun Kim
Korean Journal of Adult Nursing.2020; 32(1): 10. CrossRef - Factors Related to Self-care in Patients with Type 2 Diabetes
Seung-Yeon Kong, Mi-Kyoung Cho
The Open Nursing Journal.2020; 14(1): 64. CrossRef - Current status of treatment of type 2 diabetes mellitus in Ningbo, China
Tianmeng Yang, Rongjiong Zheng, Qingmei Chen, Yushan Mao
Journal of Clinical Laboratory Analysis.2019;[Epub] CrossRef - Prevalence and incidence of atherosclerotic cardiovascular disease and its risk factors in Korea: a nationwide population-based study
Hyungtae Kim, Siin Kim, Sola Han, Pratik P. Rane, Kathleen M. Fox, Yi Qian, Hae Sun Suh
BMC Public Health.2019;[Epub] CrossRef - The Effectiveness of Multidisciplinary Team-Based Education in the Management of Type 2 Diabetes
Jong Ho Kim, Yun Jeong Nam, Won Jin Kim, Kyung Ah Lee, A Ran Baek, Jung Nam Park, Jin Mi Kim, Seo Young Oh, Eun Heui Kim, Min Jin Lee, Yun Kyung Jeon, Bo Hyun Kim, In Joo Kim, Yong Ki Kim, Sang Soo Kim
The Journal of Korean Diabetes.2018; 19(2): 119. CrossRef - Physician-Directed Diabetes Education without a Medication Change and Associated Patient Outcomes
Hun-Sung Kim, Hyunah Kim, Hae-Kyung Yang, Eun Young Lee, Yoo Jin Jeong, Tong Min Kim, So Jung Yang, Seo Yeon Baik, Seung-Hwan Lee, Jae Hyoung Cho, In Young Choi, Hyeon Woo Yim, Bong-Yun Cha
Diabetes & Metabolism Journal.2017; 41(3): 187. CrossRef - Risks of borderline liver enzyme abnormalities to the incidence of impaired fasting glucose and diabetes mellitus: a 7 year follow up study of workers
Jin-Hyun Yu, Jin-Seok Kim, Mee-Ra Lee, Seong-Yong Yoon, Seong-Yong Cho, Seung-Hyun Yoo, Boo-Il Kim
Annals of Occupational and Environmental Medicine.2016;[Epub] CrossRef - Relationship Between Duration of Type 2 Diabetes and Self-Reported Participation in Diabetes Education in Korea
Jongnam Hwang, Jeffrey A. Johnson
Asia Pacific Journal of Public Health.2015; 27(2): NP311. CrossRef - Current Status of Management in Type 2 Diabetes Mellitus at General Hospitals in South Korea
Jin-Hee Jung, Jung-Hwa Lee, Jin-Won Noh, Jeong-Eun Park, Hee-Sook Kim, Joo-Wha Yoo, Bok-Rye Song, Jeong-rim Lee, Myeong-Hee Hong, Hyang-Mi Jang, Young Na, Hyun-Joo Lee, Jeong-Mi Lee, Yang-Gyo Kang, Sun-Young Kim, Kang-Hee Sim
Diabetes & Metabolism Journal.2015; 39(4): 307. CrossRef - Trend Analysis in the Prevalence of Type 2 Diabetes According to Risk Factors among Korean Adults: Based on the 2001~2009 Korean National Health and Nutrition Examination Survey Data
Young-Ju Kim, Myoung-Nam Lim, Dong-Suk Lee
Journal of Korean Academy of Nursing.2014; 44(6): 743. CrossRef - Evaluating Chronic Care of Public Health Centers in a Metropolitan City
Yong-Jun Choi, Dong-Soo Shin, Minah Kang, Sang-Soo Bae, Jaiyong Kim
Health Policy and Management.2014; 24(4): 312. CrossRef - Increasing risk of diabetes mellitus according to liver function alterations in electronic workers
Kyoungho Lee, Joohee Han, Soo‐Geun Kim
Journal of Diabetes Investigation.2014; 5(6): 671. CrossRef - The Effect of the Experience of Diabetes Education on Knowledge, Self-Care Behavior and Glycosylated Hemoglobin in Type 2 Diabetic Patients
Seung Hei Moon, Young Whee Lee, Ok-Kyung Ham, Soo-Hyun Kim
The Journal of Korean Academic Society of Nursing Education.2014; 20(1): 81. CrossRef - Current Status of Prescription in Type 2 Diabetic Patients from General Hospitals in Busan
Ji Hye Suk, Chang Won Lee, Sung Pyo Son, Min Cheol Kim, Jun Hyeob Ahn, Kwang Jae Lee, Ja Young Park, Sun Hye Shin, Min Jeong Kwon, Sang Soo Kim, Bo Hyun Kim, Soon Hee Lee, Jeong Hyun Park, In Joo Kim
Diabetes & Metabolism Journal.2014; 38(3): 230. CrossRef - Effect of Self-Monitoring of Blood Glucose Based Diabetes Self-Management Education on Glycemic Control in Type 2 Diabetes
Kang Hee Sim, Moon Sook Hwang
The Journal of Korean Academic Society of Nursing Education.2013; 19(2): 127. CrossRef - Diabetes Epidemics in Korea: Reappraise Nationwide Survey of Diabetes "Diabetes in Korea 2007"
Ie Byung Park, Jaiyong Kim, Dae Jung Kim, Choon Hee Chung, Jee-Young Oh, Seok Won Park, Juneyoung Lee, Kyung Mook Choi, Kyung Wan Min, Jeong Hyun Park, Hyun Shik Son, Chul Woo Ahn, Hwayoung Kim, Sunhee Lee, Im Bong Lee, Injeoung Choi, Sei Hyun Baik
Diabetes & Metabolism Journal.2013; 37(4): 233. CrossRef - Total Energy Intake May Be More Associated with Glycemic Control Compared to Each Proportion of Macronutrients in the Korean Diabetic Population
Hye Mi Kang, Dong-Jun Kim
Diabetes & Metabolism Journal.2012; 36(4): 300. CrossRef - Effect of Soybeans, Chungkukjang, and Doenjang on Blood Glucose and Serum Lipid Profile in Streptozotocin-induced Diabetic Rats
Ah-Ra Kim, Jae-Joon Lee, Sun-Sook Cha, Hae-Choon Chang, Myung-Yul Lee
Journal of the Korean Society of Food Science and Nutrition.2012; 41(5): 621. CrossRef - Comparative Study on Self-Care Behavior, Diabetes-related Stress, and Stress Coping among Good, Inadequate, and Poor Glycemic Control Groups
Hye-Yeon Kang, Mee-Ock Gu
Journal of Korean Academy of Fundamentals of Nursing.2012; 19(2): 168. CrossRef - Education as Prescription for Patients with Type 2 Diabetes Mellitus: Compliance and Efficacy in Clinical Practice
Mi Yeon Kim, Sunghwan Suh, Sang-Man Jin, Se Won Kim, Ji Cheol Bae, Kyu Yeon Hur, Sung Hye Kim, Mi Yong Rha, Young Yun Cho, Myung-Shik Lee, Moon Kyu Lee, Kwang-Won Kim, Jae Hyeon Kim
Diabetes & Metabolism Journal.2012; 36(6): 452. CrossRef - Biological Effect of Vaccinium uliginosum L. on STZ-induced Diabetes and Lipid Metabolism in Rats
Eun-Kyung Han, Hyuck-Se Kwon, Se-Gye Shin, Yoon-Hee Choi, Il-Jun Kang, Cha-Kwon Chung
Journal of the Korean Society of Food Science and Nutrition.2012; 41(12): 1727. CrossRef - Comparative Study on HbA1C, Self-care Behavior, and Quality of Life by Depression Status in Type II Diabetic Patients
Young-Min Jeong, Mi-Young Kim
Journal of Korean Academy of Fundamentals of Nursing.2012; 19(3): 353. CrossRef - Therapeutic Target Achievement in Type 2 Diabetic Patients after Hyperglycemia, Hypertension, Dyslipidemia Management
Ah Young Kang, Su Kyung Park, So Young Park, Hye Jeong Lee, Ying Han, Sa Ra Lee, Sung Hwan Suh, Duk Kyu Kim, Mi Kyoung Park
Diabetes & Metabolism Journal.2011; 35(3): 264. CrossRef - Bowl-Based Meal Plan versus Food Exchange-Based Meal Plan for Dietary Intake Control in Korean Type 2 Diabetic Patients
Hee-Jung Ahn, Boo-Kyung Koo, Ji-Yeon Jung, Hwi-Ryun Kwon, Hyun-Jin Kim, Kang-Seo Park, Kyung-Ah Han, Kyung-Wan Min
Korean Diabetes Journal.2009; 33(2): 155. CrossRef - An Evaluation of Sampling Design for Estimating an Epidemiologic Volume of Diabetes and for Assessing Present Status of Its Control in Korea
Ji-Sung Lee, Jaiyong Kim, Sei-Hyun Baik, Ie-Byung Park, Juneyoung Lee
Journal of Preventive Medicine and Public Health.2009; 42(2): 135. CrossRef - The Current Status of Type 2 Diabetes Management at a University Hospital
Young Sil Lee
Korean Diabetes Journal.2009; 33(3): 241. CrossRef - The Effect of Gamma-Glutamyltransferase on Impaired Fasting Glucose or Type 2 Diabetes in Korean Men
Tae-Yeon Kim, Do-Hoon Kim, Chang-Hae Park, Kyung-Hwan Cho, Seung-Hwan Lee, Hyuk Ga, Hwan-cheol Kim
Korean Diabetes Journal.2009; 33(3): 215. CrossRef - Management of Diabetic Mellitus in Low-income Rural Patients
Hye-Yeon Kim, Woo-Jun Yun, Min-Ho Shin, Sun-Seong Kweon, Hye-Ran Ahn, Seong-Woo Choi, Young-Hoon Lee, Dong-Hyeok Cho, Jung-Ae Rhee
Journal of Preventive Medicine and Public Health.2009; 42(5): 315. CrossRef - The Effect of Smoking Status upon Occurrence of Impaired Fasting Glucose or Type 2 Diabetes in Korean Men
Chang-Hae Park, Hyuk Ga, Jong-Han Leem, Seung-Min Kwak, Hwan-Cheol Kim, Ji-Ho Choi
Journal of Preventive Medicine and Public Health.2008; 41(4): 249. CrossRef
- Developing a nomogram for predicting depression in diabetic patients after COVID-19 using machine learning

 KDA
KDA
 First
First Prev
Prev





